 By Jim Tate, EMR Advocate
By Jim Tate, EMR Advocate
MACRA/MIPS Subject Matter Expert
Twitter: @jimtate, eMail: jimtate@emradvocate.com
Host of The Tate Chronicles – #TateDispatches
2017 was the first reporting year for MACRA/MIPS (Quality Payment Program). Only recently has it been possible to begin the deeper analysis of the data generated out of that year. We are now able to go to the CMS website, Physician Compare, to see some of the publicly reported data. However, the single most import data, the final MIPS score, is buried in data bases. That data can be accessed but not too many folks are going to examine gigantic spreadsheets to get at that data. The spreadsheet for individual MIPS eligible clinicians has over 400,000 rows. You might want to add a little RAM to your computer to play with that data.
The MACRA/MIPS program is complex, much more so than the Meaningful Use program. Since it is also a zero-sum reimbursement scheme, funds are shifted from providers with low scores to those that score high. My concern has always been that small practices would not have the administrative resources to manage the program in comparison to larger or hospital affiliated practices. The playing field would not be level. Resources and program modifications have been created to support small practices (i.e. the Small, Underserved, and Rural Support initiative) but has it been enough? The data says “no”.
CMS, in their 2017 Quality Payment Program Reporting Experience report, states that “1,057,824 clinicians were eligible for MIPS in 2017. Of these, 1,006,319, or 95 percent, participated in the program and avoided a negative payment adjustment by receiving at least 3 points as their MIPS final score.” Sounds pretty good, but let’s break down that claim. In the charts below we see that the participation rate of all MIPS eligible clinicians was 95% in 2017. For clinicians in small practices the participation rate was 81%.
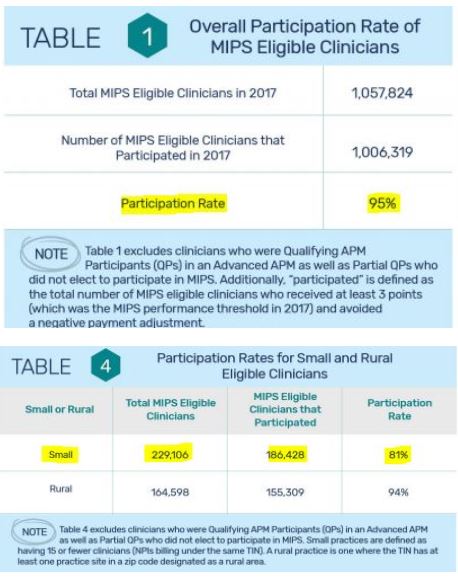
The rate of non-participation in 2017 was 380% higher for small practices compared to all MIPS eligible providers. Non-participation brought an automatic 4% negative reimbursement adjustment that took effect in 2019. To avoid that penalty would only have required the most minimum effort such as “reporting one quality measure for one patient in 2017”. Five minutes of effort in 2017 would have avoided a 4% penalty in 2019 but 42,678 MIPS eligible clinicians did not do it. The minimum requirements to avoid the increasing negative reimbursement percentages are continuing to be raised. Will the small practices continue to be left behind due to the dynamics of the MACRA/MIPS program? One year of data does not show a trend but it does show that increased effort must be made to not leave these small practices behind.
This article was originally published on MIPS Consulting Blog and is republished here with permission.
