 By David Harlow, JD MPH, Principal, The Harlow Group LLC
By David Harlow, JD MPH, Principal, The Harlow Group LLC
Twitter: @healthblawg
Host: HIPAA Chat!
The President declared an opioid abuse public health emergency recently, but the vehicle he used for the emergency declaration meant that it came with no funding, no added treatment resources, no naloxone, no expanded counseling capacity, no mandate for use of different treatment modalities. In short, a public statement without much behind it. He suggested many things in his accompanying announcement: funding, promotion of development of new pharmaceuticals, and interestingly and very specifically, a proposed waiver of a rule barring use of Medicaid funds for certain related services — though frankly, given the concurrent GOP budget efforts that include a near-trillion-dollar Medicaid cut, such a gesture is all but meaningless.
More generally, folks close to the issue don’t expect the President to come through. The commission chaired by Chris Christie — impaneled months ago, after the President first said he was going to declare an opioid abuse emergency — is due to issue a report sometime soon; perhaps it will issue cogent recommendations that may be put in place by the administration. (Of course, since it was due out within a week of the long-delayed declaration of emergency, why not just wait a week and issue a declaration with more meat on the bones?) Whether or not the panel comes up with some viable solutions, panel members don’t believe the administration will follow through on its recommendations.)
Timed to coincide with the declaration, OCR issued a new HIPAA guidance document relating to patients dealing with opioid addiction. It really doesn’t say anything new — it just confirms that, as the HIPAA rules have long provided: the best interests of the unconscious patient are often served by sharing health information with friends and family (though when the unconscious patient comes to and is competent, that decision is to be revisited); family and friends should be “read in” by health care providers when a patient poses a serious threat to his own health or safety; anyone who is a “personal representative” of a patient under state law has the right to patient information that would otherwise be private to the patient. (Nothing new here, though I learned through informal conversations with folks in the field that this guidance document was perceived in some quarters as a new regulation issued in order to deal with the opioid crisis.)
There are many efforts underway to fight the opioid crisis across our fifty laboratories, and the need is acute, with between 90 and 100 opioid-related deaths daily.
While there is often great emphasis put on making naloxone (an opioid overdose antidote) more widely available, research findings announced today point to the danger in relying on a “miracle drug” as the one-stop solution to a much more intractable problem. Looking at 30 months’ experience (ending 2015) in Massachusetts, researchers found that over 400 naloxone doses were administered per month statewide. Overall, the study concluded:
[D]espite the increased availability of naloxone — a medication that blocks or reverses the effects of opiate overdose — about 10 percent of patients treated with naloxone had died within a year of treatment. Half of those who died did so within one month of treatment. The study, conducted in Massachusetts, found that of patients treated with naloxone who died within one year of treatment, about 40 percent died outside the hospital.
“Patients who survive opioid overdoses are by no means ‘out of the woods,’” said lead study author Scott Weiner, MD, FACEP, assistant professor at Harvard Medical School and director of the Brigham Comprehensive Opioid Response and Education Program at Brigham and Women’s Hospital in Boston, Mass. “These patients continue to be at high-risk for overdose and should be connected with additional resources such as counseling, treatment and buprenorphine.”
See more in the ACEP presser released on October 30th and in the infographic reproduced below:
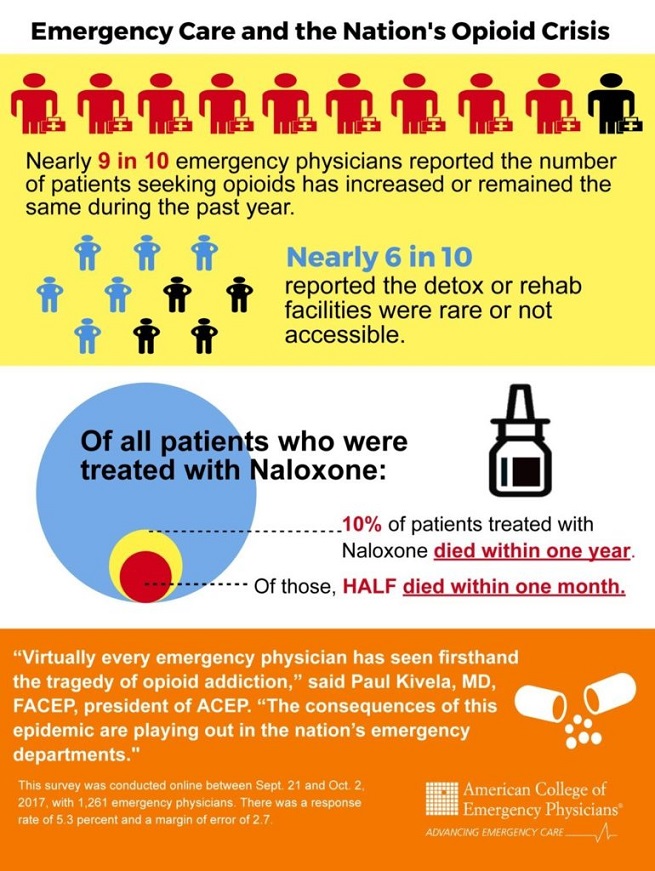
Emergency Care and the Nation’s Opioid Crisis (PRNewsfoto/American College of Emergency P)
Given the urgency of the need across the country, it is critical that the federales step up to the plate and engage in system-wide supports for multiple responses to the opioid crisis. The costs associated with failure to act decisively are too high.
This article was originally published on HealthBlawg and is republished here with permission.
