What are the Strategic IT Choices?
What are the Strategic IT Choices?
By John Halamka, MD
Twitter: @jhalamka
During my 16 years as CIO, I’ve witnessed the transition from client server to web, from desktops to mobile, and from locally hosted to cloud. As Beth Israel Deaconess merges and acquires more hospitals, more practices and more care management capabilities, what are its strategic IT choices?
I will not even mention “best of breed”, because I think the industry has abandoned such a strategy as unworkable in an era when everyone needs access to everything for care coordination, population health, and patient/family engagement.
The choices are basically two:
A. Single monolithic vendor application for everyone everywhere
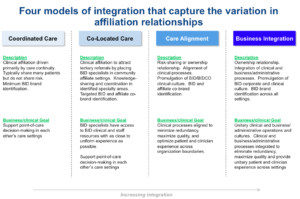
B. Best of Suite – the smallest number of applications/modules that meet the need for business integration (defined in the graphic below)
It’s extremely popular among academic medical centers, ACOs, and healthcare systems to choose “A”, often at great cost.
BIDMC has a 30 year tradition of building and buying systems balancing costs, agility, and functionality.
As I plan for the next generation of IT systems, I favor “B” and believe I can achieve our business goals in shorter time, at lower cost, with less risk.
Here’s the thinking.
- At BIDMC, we need a web-based, mobile friendly, cloud hosted solution that has the agility to support rapidly evolving research, education, and clinical requirements. The culture at BIDMC is not top down, command/control, willing to compromise but bottom up, collaborative, and impatient for innovation. We will continue to build the core clinical systems at BIDMC until there is a vendor application that meets the cultural requirements and is affordable.
- At all other sites, we will use cloud hosted inpatient and ambulatory vendor-based systems that are aligned with the business requirements and culture of the institutions.
- Our budgets are very limited to serve 22,000 users and 3000 doctors. Operating budgets for IT are 1.9% of the total spend. Capital is about $10 million a year. One time capital for major IT initiatives is unlikely to ever exceed $20 million. When I hear about expenditures of hundreds of millions for IT systems, I really wonder how the economics are sustainable.
- Interoperability for care coordination across a small number of applications is possible via bidirectional viewing, pushing summaries, and pulling records via the state healthcare information highway.
- Business intelligence/analytics across the network is supported by financial and clinical registries, populated via well described interfaces.
Over the next 90 days stakeholders from throughout the organization will complete the next generation IT plan as follows:
- July – strategy complete, draft budgets submitted
- August – organizational structure for unified enterprise IT proposed, budgets finalized
- September – staffing plan finalized and timelines aligned for execution beginning October 1
As with any plan, change management will be the most challenging aspect, balancing time, resources, and scope.
Over the coming months, I’ll share the decisions we’ve made for a cloud of community hospital functionality and a cloud of ambulatory EHR functionality that unifies all our practices.
John D. Halamka, MD, MS, is Chief Information Officer of Beth Israel Deaconess Medical Center, Chairman of the New England Healthcare Exchange Network (NEHEN), Co-Chair of the HIT Standards Committee, a full Professor at Harvard Medical School, and a practicing Emergency Physician. This article was originally published in his blog Life as a Healthcare CIO and is reprinted here with permission.