
By Rich Rutherford, President and General Partner, Project Navigation
Twitter: @proj_navigation
Aligning incentive and quality programs with existing Accountable Care Organization (ACO) agreements is essential to improving patient outcomes and confidently negotiating private payer risk-based contracts. I started installing EHRs in 1999 with expected benefits of prescription legibility and reduced chart pulls. Today’s EHR has a similar impact to medicine as that of the electrocardiogram (EKG) in 1903. Electric pulses display patterns to determine heart health and EHRs capture electric data patterns for a population to assess and manage the health of our communities. Population Health is dependent on EHR data and evidence-based interventions to ensure the population is stratified accurately. Nobody argues the benefit of being able to track results for improvements as this is a benchmark in all industries. The strategy providers and hospitals execute will determine who is providing services five years from now. The five steps below are critical to establishing this strategy.
1. Crosswalk Program Measures Utilizing the National Quality Forum (NQF) Number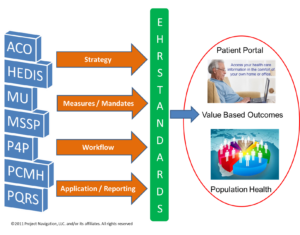
a. Building a crosswalk is an exercise that defines like measures across ACO contracts, incentive and quality programs. Pick a baseline program to draw measure correlations to the other programs. We recommend utilizing the NQF number as the common thread among these programs; however, not every measure within each program has a NQF number. In addition, not every program uses the same measure subset nor are all measures applicable to each medical specialty or to your business.
b. The objective of the crosswalk is to determine the measure pool for which supports the achievement of all programs by providers as a byproduct of providing good quality care.
2. EHR Capability and Reporting
a. With the measure pool proposed, it is time to confirm that the EHR will support the measures selected. This includes software versions, application configuration and data submission capability for each program targeted.
b. Capturing quality measures from claims data is a short term and short-sited strategy. Only evidence-based content collected in the EHR has the ability to improve the patient’s outcome at the point of the encounter.
c. The EHR content captured is the foundation that population health software will use for risk stratification. The measure pool should be aligned to the risk factors defined in the community assessment. This ensures that measures and community health management are in aligned to have the largest impact in patient outcomes in the community.
3. EHR Workflow, Training and Dashboards
a. Once the measure pool is finalized, workflow and training material need to be updated to include steps to capture the necessary documentation. Documentation that is not captured consistently on the patient population will result in ineffective risk stratification and quality measure degradation.
b. Physician dashboards or reports must be available to track performance and remediation plans. Since quality data has been reported from claims historically, the right tools and feedback loops to the healthcare team has been lacking.
4. Provider Alignment
a. The patient determines the hospital or physician they will use for health services based on quantified quality data available on hospital and physician compare CMS websites. This information is publicly available to software developers through APIs so shopping for healthcare services based on reviews will become as common as reviewing products on Amazon.
b. Patient volume, and therefore revenue, will be driven by patients armed with subjective patient reviews and quantitative quality outcomes based on the services they are seeking.
c. On January 26, 2015, the U.S. Department of Health & Human Services aligned patient outcomes to Medicare payments stating “HHS has set a goal of tying 30 percent of traditional, or fee-for-service, Medicare payments to quality or value through alternative payment models, such as Accountable Care Organizations (ACO) or bundled payment arrangements by the end of 2016, and tying 50 percent of payments to these models by the end of 2018”. (HHS Press Office, 2015)
d. Provider operating contracts need to include incentives now for quality outcomes to shape behavior in preparation for the fee for value transition in 2016 for Medicare, which will be quickly followed by the private insurance industry.
5. Governance Change Control
a. A robust governance structure with change control process is necessary more than ever before. The effort put forth to improve outcomes can be lost when introducing new applications, workflows and existing application change requests. Detailed change control process for checking baseline measures and workflows are required.
b. A test environment reflecting production with reporting capability ensures that impacts to outcomes are mitigated through testing before we affect the care of our patients.
Please send me your comments as we navigate the “fee for value” transition in healthcare. rich.rutherford@projectnavigation.com
This article was originally published on Project Navigation and is republished here with permission.
