 By Tom Dorsett, CEO, RazorMetrics
By Tom Dorsett, CEO, RazorMetrics
Twitter: @razormetrics
Drug costs are skyrocketing, but why? This is an essential question to ask since we must understand the cause of high drug costs in order to properly address the problem. As someone who has worked in healthcare and life sciences technology for more than twenty-five years, I’ve seen drug costs grow and dominate pharmacy budgets across the United States. Despite substantial technological improvements during this period, drug prices remain unaffordable for many Americans. After extensive contemplation, I’ve concluded that the root causes of high drug costs fall into five categories.
#1 Research and development costs are recouped through drug prices.
It should come as no surprise that pharmaceutical companies always point to R&D as the number one reason the final price of their new drug is high. They are recouping their investment into the drug but also trying to cover the losses of other drugs that failed in the testing phase.
The average time to bring a drug from ideation to market is about 10-15 years, according to the industry group PhRMA. Many things can go wrong during the process, from initial efficacy testing to clinical trials, regulatory approvals, and finally, reaching new patients. Ten to fifteen years is a big commitment to make on something that might not pan out. Eighty percent of clinical trials fail to meet their enrollment objectives making things even more challenging.
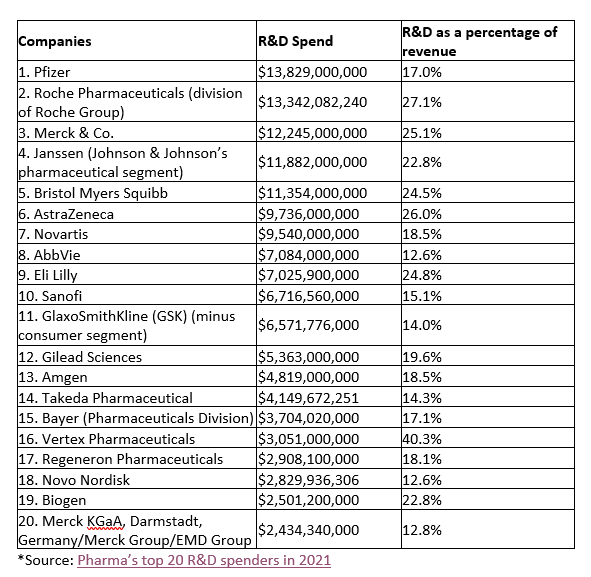
Pharmaceutical companies spend billions of dollars each year on R&D, which sounds like a lot. However, when looking at the R&D spend as a percentage of their revenue, it doesn’t look as impressive. There is no set rule in finance on how much is best to reinvest in a company’s core business; some experts say 50% of profits, while others recommend 20%. Thirteen of the world’s 20 biggest pharma spenders reinvest less than 20% of their revenue in creating new treatments.
Nevertheless, the R&D budgets are passed onto consumers through higher drug prices on all their brand-name drugs. As research budgets increase, so do the cost of currently available medications to cover those costs.
#2 Drug patent rules provide 14.5 years of exclusivity on average.
Harvard Medical School reviewed U.S. pharmaceutical laws and regulations establishing exclusivity periods for drug manufacturers. An exclusivity period bars any other manufacturer from making a generic version of their patent-protected drug. Researchers found that manufacturers can extend their 10-12 year patent protection in several ways:
- applying for more patent time (up to five years) during the clinical trial period;
- conducting trials in children gives an additional six months of exclusivity; and
- obtaining secondary patents on the drug’s manufacturing methods.
Brand name drugs and their generic counterparts are chemically exact and cost about the same to manufacture, but the price to consumers can differ by thousands of dollars a month. The longer a company can stave off competition from generics, the more revenue they make off the patent. The consequence of this delay is that the average American can only afford drug technology that is 10-15 years old.
#3 Inflation in drug prices outpaced inflation in other sectors.
Everything is more expensive, so it makes sense that inflation impacts drug manufacturing as well. But that doesn’t explain why inflation in prescription drug prices outpaced the rise in gas, food, tuition, utilities, car prices, and personal care items. The difference is stark: from 2014 to 2021, the cost of goods and services increased by 19%, while prescription drug prices increased by 35%.
One reason for this was that manufacturers increased the price of certain drugs by 300% or more because they believed the market would pay it, not due to any resource price increases. There is no law against rapidly increasing the price of a monopolized drug product, even one that is life-dependent for many people, like insulin.
#4 Manufacturing has become more complex.
New medicine development technology has dramatically increased the complexity of manufacturing. One example is Biologics, medicines made from living organisms, and the process of making these is delicate. The complexity has increased the cost of manufacturing and limited the ability of others to make a cheaper version once the patent runs out. This situation is changing, though, due to the rise of biosimilars, which are therapeutically exact but not chemically. Biosimilars must go through a more rigorous FDA testing protocol than traditional generics, and this adds to their cost, but they are much less expensive than the name-brand versions.
#5 Negotiated drug prices are under-utilized.
A lot of work goes into negotiating lower prices with pharmaceutical manufacturers. Health plans and self-funded employers and their PBMs spend significant time creating their formularies, a list of approved drugs that are more affordable for their members/employees. The problem is that once this formulary is released into the wild, there is little control over what is actually prescribed.
One of the most significant sources of excess pharmacy spend is due to prescribers. The overspending is unintentional, of course. Physicians prescribe the drugs they know, not the ones on each patient’s insurance formulary. Technology companies have tried to bridge this knowledge gap with Real-Time-Benefit-Tools with very limited success because the technology takes physicians out of their everyday workflow and the data provided at the point-of-care lacks reliability. Other solutions have shifted the burden of prescribing onto the patients by requiring them to research possible drug alternatives in an app or a website. The best solution relies on the person with the most knowledge about the patient’s health and needs and who has the authority and responsibility to write prescriptions – the prescriber.
In my years of experience, the cost of medicine is complex, but the solution doesn’t have to be. People have access to affordable drugs through their insurance; it just takes the prescriber to match the right treatment option with the patient.
