 By Kathryn Marchesini, Jeff Smith, and Jordan Everson, ONC
By Kathryn Marchesini, Jeff Smith, and Jordan Everson, ONC
Twitter: @ONC_HealthIT
The same basic technology that can predict what movie you might want to watch, what song you might want to listen to, or what item you might want to buy online, can also predict the onset of diseases, forecast costs of care, and recommend treatment options for your doctors, nurses, and pharmacists.
Algorithms are not new to health care. Indeed, an important and long-standing part of our Health Information Technology (Health IT) Certification Program has included Clinical Decision Support (CDS) certification criterion covering “rules-based” algorithms and software systems that use rules derived by experts, such as clinical guidelines, to turn “inputs” into an “output.” While decision support technologies have existed for decades (and will be the subject of a forthcoming blog series), the application of artificial intelligence (AI) and machine learning (ML) to decision-making has been steadily growing. So too has the scale and volume of the data used to power these new computing technologies. Not a day goes by where we don’t read about a new study, product, or application of AI/ML to aid decision-making in health care settings, such as predicting pneumonia in the emergency department, predicting inpatient mortality, and assisting clinicians in diagnosing hip fractures, just to name a few.
These technologies have the potential to drive innovation, increase market competition, and vastly improve care for patients and populations. However, like any new health IT, it requires examination and inquiry to establish an evidence-base of benefits and risks. What we know from studies to date is that AI/ML-driven predictive technology may positively or negatively impact patient safety, introduce or propagate bias, and result in increased or reduced costs. In short, results have been mixed. But the interest—and potential benefit—remains high.
In order to motivate deeper discussion about the appropriate use of these new and evolving technologies, the Office of the National Coordinator for Health Information Technology (ONC), within the U.S. Department of Health and Human Services (HHS), has been convening stakeholders working with AI/ML technologies through public events such as our AI showcase, a Health Information Technology Advisory Committee hearing on algorithmic bias, and session on equity and algorithms at our annual meeting. ONC is also actively monitoring and engaged in health and AI-focused initiatives such as the Coalition for Health AI and in a number of cross-agency coordination efforts with our federal partners.
We are on the cusp of what will be a long-term trend of combining health data with complex predictive models and algorithms to improve diagnosis, treatment, and care management of patients and populations. ONC-certified health IT increasingly serves as the wellspring for algorithms, providing data and tools for the creation of algorithms in health care, and as the delivery mechanism 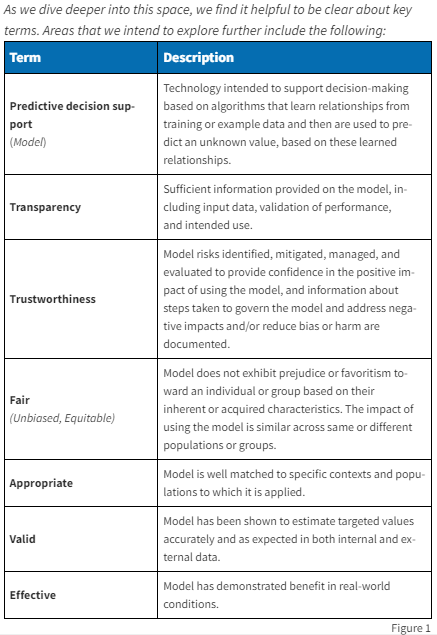 of algorithms, inserting algorithmic results and outputs into clinical and administrative decision-making. Facilitating the use of these emerging technologies in ways that maximize their benefits and minimize their negative unintended consequences is thus of high importance to ONC and HHS.
of algorithms, inserting algorithmic results and outputs into clinical and administrative decision-making. Facilitating the use of these emerging technologies in ways that maximize their benefits and minimize their negative unintended consequences is thus of high importance to ONC and HHS.
Stay Tuned, More to Come
This is the first in a series of blog posts where we’ll discuss the current and future state of algorithms and emerging technologies used to aid decision-making in health care. Through this series, we intend to provide more on the perspectives from ONC and stakeholders on this evolving space, including in the context of health equity by design approaches to promote “fair, appropriate, valid, and effective” predictive models in health care.
This article was originally published on the Health IT Buzz and is syndicated here with permission.
