 By Jeremy Guttman, Researcher and Content Developer, Treatspace
By Jeremy Guttman, Researcher and Content Developer, Treatspace
Twitter: @Treatspace
In almost every speech given this year, Andy Slavitt, the Acting Administrator for the Centers for Medicare and Medicaid Services (CMS), has emphasized the priority of closing referral loops to strengthen patient care coordination.
Independent practices have less than a year to prepare for newly developed value-based care reimbursement guidelines. However, many practice leaders are struggling to find an efficient way to close referral loops. Closed-loop referral management is achieved when a primary care physician can both analyze and track what happens with every patient at every step of the referral process when a patient is referred to a specialist.
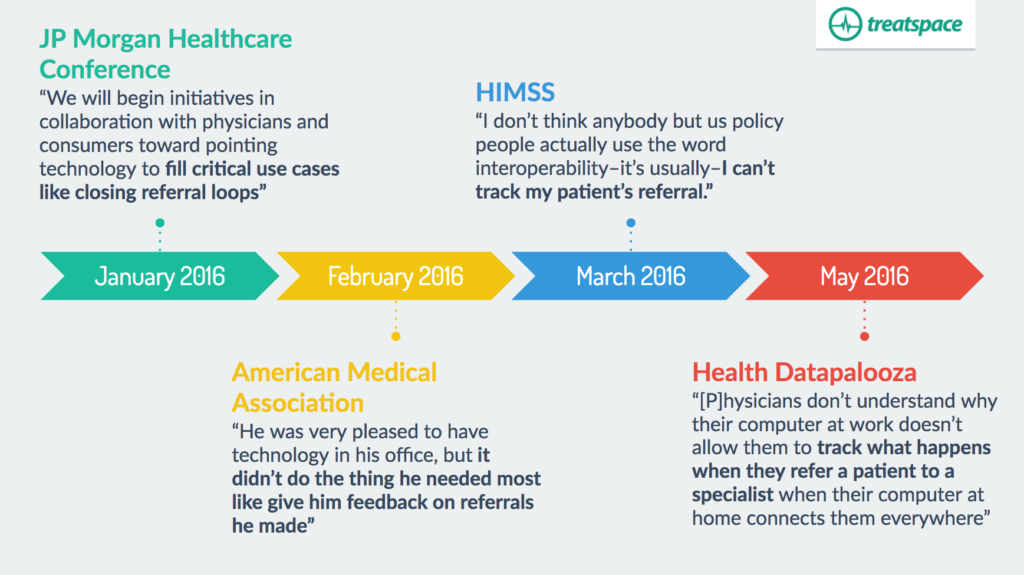
Below we detail four of Andy Slavitt’s recent speeches where referral management was highlighted as a critical path to follow for the future of interoperability and to meet the requirements of physicians today.
Highlighting referral management and redefining Meaningful Use
– speaker at JP Morgan Healthcare Conference [Jan 2016]
In January 2016, Slavitt gave a widely reported speech at the JP Morgan Healthcare Conference where he declared that “[t]he Meaningful Use program as it has existed will now be effectively over.” The later stages of the Meaningful Use program became somewhat controversial because many felt that the program did not focus enough on practical outcomes for patients. A number of healthcare leaders and organizations were calling for the program to be fixed or eliminated in late 2015 and early 2016. Andy Slavitt’s January 2016 speech was a response to the rising tide of complaints about the program.
To illustrate how to focus more on practical patient outcomes, Slavitt highlighted the need to close referral loops:
“[W]e are deadly serious about interoperability. We will begin initiatives in collaboration with physicians and consumers toward pointing technology to fill critical use cases like closing referral loops.”
In a blogpost soon afterwards, he reiterated how critical it is to be “focusing on real-world uses of technology, like ensuring continuity of care during referrals.” Some closed-loop referral initiatives have been incorporated into proposed details of the new Medicare reimbursement model passed in 2015, called MACRA. In the coming years, additional initiatives will reward physician practices for closing referral loops.
Confronting referrals lost in transition
– “Administration’s perspective” speaker at American Medical Association National Advocacy Conference [Feb 2016]
In his February AMA speech, Slavitt mentioned how care coordination and “all the transitions where people get lost” were some of the areas the government needs to invest in to keep doctors fully informed about their patients.
His example was a story of a physician who was “very pleased to have technology in his office, but it didn’t do the thing he needed most like give him feedback on referrals he made.” [emphasis in original]
Nationwide, physicians pinpoint closing referral loops
– “A Special Session with ONC and CMS” panel discussion at HIMSS16 [March 2016]
Andy Slavitt discussed physicians’ desire for referral tracking on a panel discussion at the Healthcare Information and Management Systems Society (HIMSS) 2016 conference in Las Vegas. He said that when CMS conducted numerous physician focus groups and workshops across the country earlier this year, physicians from those groups reported that closing the referral loop was one of their most important needs.
Problems with interoperability often equated to “I can’t track my patient’s referral.”
Because of this physician feedback, the government has agreed to further promote closing referral loops in new legislation.
Currently, tracking referrals is impossible
– keynote speaker, Health Datapalooza [May 2016]
Here, Andy Slavitt highlighted the physician data paradox, where physicians are overloaded with data entry tasks but all of that data can’t be put together to inform physicians with useful, important and actionable information.
Physicians are “overloaded on data entry and yet rampantly under-informed…And physicians don’t understand why their computer at work doesn’t allow them to track what happens when they refer a patient to a specialist when their computer at home connects them everywhere.”
This physician data paradox is a direct result of the limitations of electronic health record (EHR) systems. EHRs gather massive amounts of data, but still don’t do enough for physicians to achieve what they truly want for optimal care for their patients: referral management.
Follow Andy Slavitt’s Lead
We are in the middle of one of the biggest shifts in healthcare reimbursement methods in history. CMS is leading the charge in changing financial incentives to reward value-based primary care. And they’re not slowing down. When physicians are asked what they want from technology, they respond loud and clear: they want to track patient referrals.
As more influential legislators recognize the importance of tracking and closing referral loops, high-performance referral management is set to become a priority for practices who want to stay competitive.
Is your practice currently managing care transitions and closing the loop on patient referrals?
This article was originally published on Treatspace and is republished here with permission.
