By Eliana Donner-Klein, Senior Associate for Marketing & Michelle Rubin, Senior Manager, Audacious Inquiry
By Eliana Donner-Klein, Senior Associate for Marketing & Michelle Rubin, Senior Manager, Audacious Inquiry
Twitter: @A_INQ
Health disparities are a long-standing challenge in the United States and worldwide. In light of the COVID-19 pandemic and its higher impact on vulnerable and marginalized groups, more attention is being directed towards achieving health equity. With a focus on the relationship between health, social factors, and their role in public health, researchers, policy makers and the public at large have noticed and documented health disparities between a range of population groups.
The health information technology field has progressively recognized that addressing health disparities to achieve health equity needs to be a cross-sector effort. Yet, there is still groundwork to be done to raise awareness about the differences between health equity, health disparities and the social determinants of health, how health disparities affect different populations around the country, and how healthcare organizations and entities can work to begin addressing health equity. More specifically, this blog will identify some of the key areas for health IT organizations and professionals to make a measurable impact in improving health equity by promoting the consistent collection of health equity data and evaluating how health IT software can support data exchange and analytics to improve patient care and public health policy development at the local, state, and federal levels.
What is the Difference between Health Equity and Social Determinants of Health?
Health equity and social determinants of health, while related, are often used interchangeably. The Centers for Disease Control and Prevention (CDC) defines health equity as when every person has the opportunity to “attain their full health potential” without being “disadvantaged from achieving this potential because of their social position or other socially determined circumstance.” Achieving health equity requires removing obstacles to health like poverty and discrimination that adversely affect excluded or marginalized groups to provide better access to healthcare.
The social determinants of health, on the other hand, are conditions in the places where people learn, live, and work that affect health and quality of life and health outcomes. Addressing the social determinants of health is an approach to achieving health equity.
What are Examples of Health Disparities?
Health disparities are defined as “preventable differences in the burden of disease, injury, violence, or opportunities to achieve optimal health that are experienced by socially disadvantaged populations.” The key word in this definition is “preventable.” These disparities include life expectancy, access to healthcare, morbidity, and mortality, and can manifest differently for various populations.
Health disparities can be seen in many aspects of healthcare and health outcomes. Asthma is a chronic disease that has a higher prevalence for multiple socially disadvantaged populations, including women, multiracial, American Indian, Alaska Native, Hawaiian, and Pacific Islander adults compared with white adults. According to the Asthma and Allergy Foundation of America, Black Americans are 1.5 times more likely to have asthma, 5 times more likely to visit the emergency department due to asthma, and 3 times more likely to die from asthma. Beyond race, asthma is more prevalent among adults with a high school or lesser education than college graduates and adults with an annual income of $25,000 or less compared to those with higher income levels. Asthma can be controlled using inhalers and other therapeutics; yet access to healthcare, insurance coverage, and lack of education on environmental triggers, present challenges in treating severe asthma and reducing asthma-related deaths, hospitalizations, and emergency department visits.
Health disparities also exist beyond racial and ethnic categorization but can be difficult to identify and measure. Many public health surveys and health care providers do not generally ask about other demographic characteristics, like sexual orientation and gender identity questions. Gay and bisexual men, especially those who are young and people of color, have higher risk of HIV and other STIs than other populations. Additionally, lesbian women are 25% less likely than heterosexual women to get timely pap spears (cervical cancer screening). According to the Office of Disease Prevention and Health Promotion, enhancing efforts to improve LGBTQ health disparities can include reductions in disease transmission and progression, increased mental and physical well-being, reduced health care costs, and increased life expectancy. Consistent collection and adoption of sexual orientation and gender identity data is needed to help accurately characterize LGBTQ health and disparities to implement effective, widespread interventions.
Health equity data has generally been under-reported due to a lack of standards to collect this information and limited adoption of reporting of health equity data in standard healthcare operations. The healthcare and public health sectors are prioritizing better collection and analysis of health equity data to identify areas of improvement and institute initiatives to reduce health disparities and improve health equity.
Current Discussions of Health Equity
The COVID-19 pandemic has brought health disparities and health equity into mainstream conversations. Headlines from across the country broadcasted statistics about higher rates of COVID-19 infection, hospitalization, and death in people of color than white people. Since January 2021, the Biden administration has renewed the federal government’s focus on health equity, promulgating a policy to “pursue a comprehensive approach to advancing equity for all, including people of color and others who have been historically underserved, marginalized, and adversely affected by persistent poverty and inequality. Affirmatively advancing equity, civil rights, racial justice, and equal opportunity is the responsibility of the whole of our government.”
The COVID-19 pandemic illustrated that data related to health equity, like race, ethnicity, and language preferences, was not consistently being recorded across the healthcare and public health systems. According to an article in Health Affairs, at the first peak of the pandemic in 2020, only 24 states had reported race and ethnicity data of people who had died from COVID-19. During the first month of vaccine distribution, race and ethnicity data were missing for 48 percent of people, even though this was required for collection. This variation in adoption has led to inconsistencies in the collection and uniformity of health equity data, like gaps in information and the inability to stratify data.
Published best practices encourage state and local leaders to disaggregate COVID-19 case data, and consistently measure access to testing and treatment and other relevant measures, by age, race, ethnicity, gender, disability, neighborhood, and other sociodemographic characteristics. Analyzing data in this way illustrates the interplay between place and social factors, allowing for informed decision-making based on a better understanding of the rate of infection, testing, and vaccinations across populations to ensure equitable access to resources. This approach should also be utilized for other healthcare data not related to COVID-19; however, challenges remain in ensuring adoption of standards and consistent inclusion in medical records.
The Office of the National Coordinator for Health IT (ONC) and CDC have both taken steps to advance health equity. The National Coordinator for Health IT, Micky Tripathi, talks about “health equity by design” whereby standards and processes explicitly consider the impact they can have on health equity. Tripathi notes that health equity considerations should be baked in as a fundamental design criterion to have a better understanding of health equity through improved reporting and analytics. Similarly, CDC director Rochelle P. Walensky called racism a “serious public health threat that directly affects the well-being of millions of Americans.”
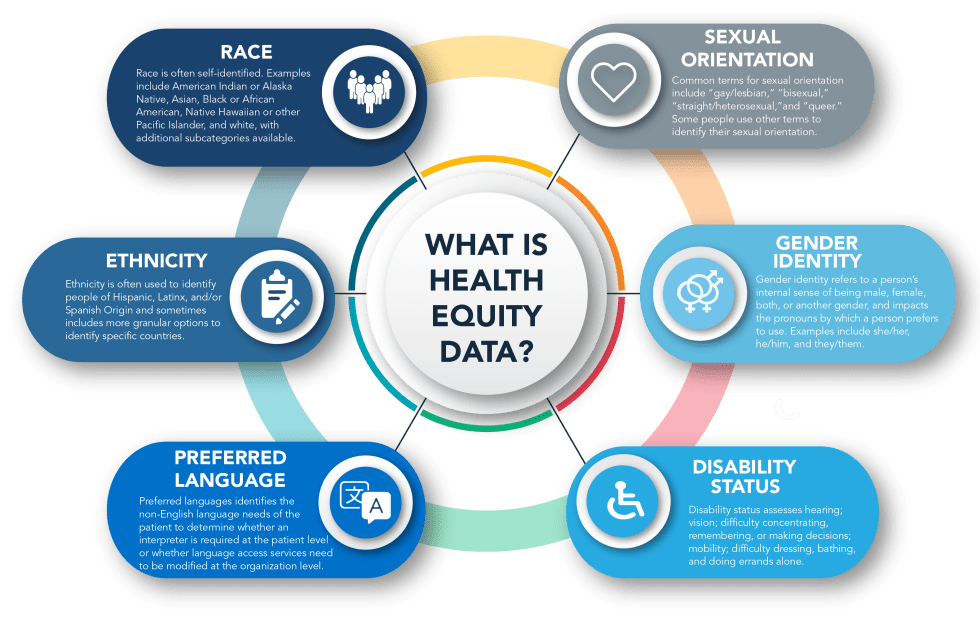
Micky Tripathi noted that addressing health equity begins with the standardized collection of health equity data. This data is key to identifying disparities, understanding why they exist, and developing and evaluating interventions. As part of its Health IT Certification Program, ONC currently requires the implementation of standards for race, ethnicity, and language. CDC also supports a data set with over 900 categories to capture race, ethnicity and language data. In July 2021, ONC announced updated interoperability standards to support the electronic exchange of sexual orientation, gender identity, and social determinants of health to help build a path forward for health IT to support exchanging this data.
Other non-governmental organizations like the Gravity Project are also identifying areas to improve data collection as evidence continues to demonstrate strong links between social risk, health and health care utilization. The Gravity Project, initiated by SIREN and the Robert Wood Johnson Foundation in 2018, seeks to create and maintain a consensus-building community to expand available social determinants of health core data for interoperability. It aims to accelerate standards-based information exchange by using HL7 FHIR to help healthcare organizations incorporate social risk data into clinical decision making to improve health outcomes and reduce costs.
The first step in standardizing the consistent collection of health equity data at the federal and industry levels is recognizing the importance of better health equity data to improve health outcomes, lower costs, and expand access to healthcare and other necessary social interventions.
The Role of Health IT in Improving Health Equity
Making strides to improve health equity and reduce health disparities cannot happen unless health IT, as the enabling mechanism of healthcare data exchange, begins to critically assess and incorporate health equity into every part of its software development process, partnerships, and policies. As highlighted throughout this blog, data is essential in uncovering and informing work to address inequities and disparities in healthcare.
Health IT provides the data standards to help ensure that data is collected uniformly across settings, and the infrastructure to support data exchange among those involved in patient care and public health policy development. With standards and exchanges in place, health IT supports a data-driven four-step approach to promoting health equity:
- Identify – Use demographic and similar data elements to understand population composition, especially as it relates to those who have been historically underserved, marginalized, and adversely affected by persistent poverty and inequality.
- Exchange – Share those data elements with others involved in the patient’s care.
- Analyze – Conduct simple and statistical analyses, alongside clinical data, to identify disparities among populations.
- Intervene – Use the analysis to develop, execute, and evaluate interventions designed to promote health equity.
Using the four steps above–identify, exchange, analyze, and intervene–health IT organizations can evaluate their role in addressing health equity and identify a roadmap to examine whether they are receiving demographic and population data from data sources.
For example, does the software include the option to document or record race, ethnicity, or language in patient records? Does the software include the option to document gender identity and preferred pronouns? If so, do workflows support ensuring data accuracy and completeness? Once collected, are there capabilities to analyze this data, the trends, and begin to identify approaches to more consistently collect health equity data—like developing resources to educate data sources on the importance of including health equity data in healthcare records?
While addressing equity may seem like an overwhelming task, it is important to remember that every person and organization can play a role by recognizing the effect of health equity, educating others who may not be aware of health equity or current health disparities, and begin to apply the data-driven four-step approach to promote health equity to software and data standards internally. Talk to your partners about their health equity efforts, and how your job as a data steward can help support their programs and services.
Ensuring that health equity data is being recorded in a uniform way with widespread adoption across the United States will lead to better insights on the health disparities that currently exist and allow for better interventions to improve health equity at a larger scale.
As the federal government continues to focus on a multi-agency plan to address health equity, health IT organizations can begin to internally evaluate their role in identifying and including health equity data in their own software and services. Additionally, public health agencies, payers, non-governmental organizations, and stakeholders have been working to improve the use of health IT to support data collection related to health equity to better inform policy and program development, clinical decisions, lower costs of unnecessary utilization, and better health outcomes. Health IT organizations have an opportunity to support tangible goals and initiatives to support this cross-sector call to achieve to achieve health equity for all Americans.
This is the first installment of Audacious Inquiry’s Health Equity blog series. As a national leader in care coordination technology, Audacious recognizes the role health IT companies can play to advance health equity and is committed to working to identify areas to address health equity.
This article was originally published on the Audacious Inquiry blog and is republished here with permission.