By Chelsea Richwine and Christian Johnson, ONC
By Chelsea Richwine and Christian Johnson, ONC
Twitter: @ONC_HealthIT
New ONC data show that, as of 2021, nearly all non-federal acute care hospitals were enabled to electronically prescribe controlled substances (EPCS).
According to the American Hospital Association (AHA) Information Technology (IT) Supplement Survey, the proportion of non-federal acute care hospitals enabled for EPCS increased from 67% in 2018 to 96% in 2021. Increased adoption of EPCS by hospitals is significant because e-prescribing enhances hospitals’ capability to ensure patient safety, avoid errors associated with paper-based prescribing, reduce prescription drug fraud and abuse, mitigate provider burden, and improve care coordination and workflow efficiency.
Moving from Paper to E-Prescribing
Health care providers have historically relied on paper-based methods to prescribe controlled substances, while those prescribing non-controlled substances have benefited from e-prescribing technologies. Decreasing reliance on paper prescriptions helps improve care coordination among providers and clinical workflow efficiencies by streamlining all prescribing into a single workflow. E-prescribing helps prevent data entry errors, reduces pharmacy calls to prescribers to clarify written instructions, and eliminates the need to coordinate and manage paper prescriptions between doctors, patients, pharmacies, and other care sites. Most importantly, e-prescribing promotes patient safety by enabling health care providers to take advantage of safety features built into health IT products that can alert prescribers of potential drug interactions, inappropriate doses, allergies, and underlying patient conditions.
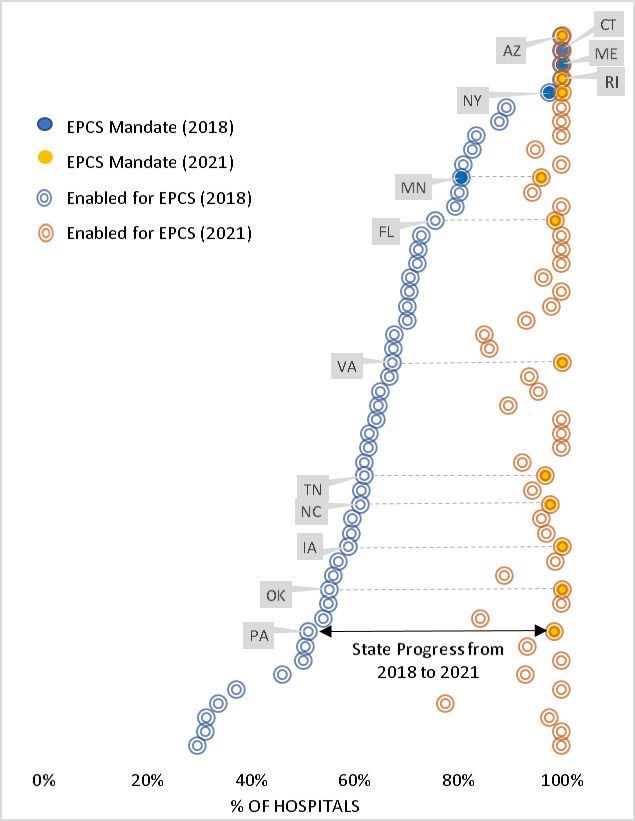
Policies at the state and federal level may have been a driving factor in the adoption of EPCS among hospitals. Following the 2010 DEA regulations that made it legal to prescribe controlled substances electronically, all states amended their laws to permit EPCS by 2015. Shortly after, the Substance Use-Disorder Prevention that Promotes Opioid Recovery and Treatment (SUPPORT) for Patients and Communities Act, enacted in 2018, required Medicare Part D prescriptions of opioids and other controlled drugs be prescribed electronically beginning in 2021. The Centers for Medicare & Medicaid Services (CMS) implemented and finalized this mandate through the Calendar Year (CY) 2021 Physician Fee Schedule. To promote widespread use of EPCS, a critical tool for improving opioid prescribing practices and combatting prescription drug fraud and abuse, thirteen states had their own mandatory EPCS laws in effect prior to 2021.
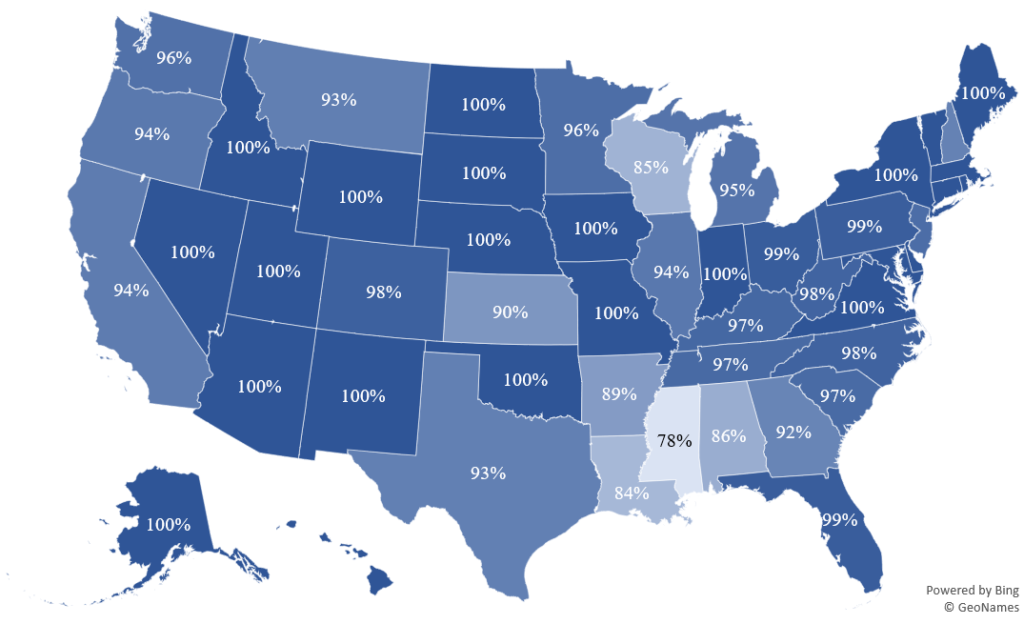
In addition to high rates of EPCS enablement observed at the national level, hospital adoption of EPCS was widespread in all states. Figure 1 shows that in half of all states, 100% of non-federal acute care hospitals reported being enabled for EPCS. In forty-five states plus the District of Columbia, more than 90% of non-federal acute care hospitals reported being enabled for EPCS. Figure 2 shows that nearly all non-federal acute care hospitals in states with mandatory EPCS laws were enabled for EPCS when data were collected in 2021.
Figure 1: Percent of non-federal acute care hospitals enabled for EPCS by state, 2021.
Data Source: American Hospital Association IT Supplement Survey
Figure 2: Change in the percent of non-federal acute care hospitals enabled for EPCS by state, 2018-2021.
Data Source: American Hospital Association IT Supplement Survey
Use of EPCS among office-based physicians is also growing, particularly among physicians who frequently prescribe controlled substances. Work continues to increase utilization of EPCS in physician practices among solo practitioners and smaller, lower-resourced practices.
A Playbook for ECPS
To aid increased adoption and use of health IT in clinical settings, ONC developed and published the Health IT Playbook, a resource for health care providers and their administrators to optimize the safety and use of their electronic health records. The Playbook also includes educational materials for health care providers about the benefits of EPCS to support the appropriate prescribing of opioids and other controlled substances, protect patients at risk for opioid misuse or abuse, and reduce fraud and drug diversion. Together, we can use health IT to support safer use and management of controlled substance prescriptions.
This article was originally published on the Health IT Buzz and is syndicated here with permission.