By Stephanie Fraser
Conference Correspondent, Answers Media Network
LinkedIn: Stephanie Fraser
Event: HIMSS 2025
When: March 2025
Where: Las Vegas NV
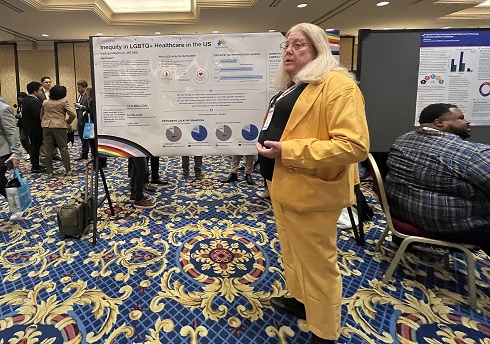
At HIMSS25, Kathryn Redman, MS MIS, an analytics expert from Saint Luke’s Health System, led a compelling discussion on the systemic inequities facing transgender and non-binary patients—barriers that contribute to delayed care, misdiagnoses, and poor health outcomes for an already vulnerable population.
With an estimated 5.3 million transgender and non-binary individuals in the U.S., 31% do not receive regular medical care, and nearly 48% report negative healthcare experiences. These statistics underscore the urgent need for better workforce training, inclusive healthcare policies, and improved EHR data tracking to ensure equitable, patient-centered care.
Healthcare’s Readiness Gap
Redman’s presentation, in partnership with Johnson County Community College in Kansas, highlighted industry’s stark knowledge gaps and the health system’s lack of readiness to address transgender health concerns, including:
- 85% of physicians lack training in transgender patient care (Mayo Clinic & Endocrine Society).
- 83% of emergency physicians have never treated or recorded data on a transgender patient (American College of Emergency Physicians).
- 88% of emergency physicians do not ask about gender identity during treatment.
Redman noted that while our healthcare system is well-equipped to treat the 2 million Americans with Type 1 diabetes, it is significantly less prepared to care for the 5.3 million transgender and non-binary individuals who require specialized medical considerations.
How EHRs are Failing
One of the most pressing issues in transgender care is the lack of a comprehensive patient health record. Many current systems only record legal sex, omitting critical EHR data such as:
- Gender identity
- Sex assigned at birth
- Sexual orientation
- Organ inventory (i.e., retained reproductive organs, prostate, etc.)
These missing fields in the EHR create risks for misdiagnosis and inappropriate treatment. For example, a transgender woman may still require prostate cancer screenings, and a transgender man may need breast cancer and cervical screenings, however without proper tracking, these critical care needs can be overlooked.
Redman proposed enhancing capture of this data to allow clinical decision support tools to generate more accurate recommendations, without making assumptions based on legal sex alone.
Collecting and analyzing gender identity data also allows public health officials to track health disparities, inform policy decisions and improve funding for LGBTQ+ health programs.
Workforce Training to Close Transgender Care Gaps
Beyond data collection, training providers on transgender and non-binary health needs is essential. Without a fundamental understanding of hormone therapy, organ retention and unique health risks, providers cannot deliver appropriate care.
Redman urged health systems to require training on LGBTQ+ healthcare competencies, integrating it into medical school curricula, residency programs and ongoing physician education.
Transgender and non-binary individuals also experience higher rates of suicide (40% attempted suicide compared to 4.5% of the general population), higher rates of substance abuse (35% vs. 11.4% of the general population), and greater exposure to intimate partner violence. Without inclusive care practices and workforce training, these risks remain unaddressed, further exacerbating health disparities.
Next Steps for Health IT Leaders
With health disparities widening, Redman emphasized that now is the time for Health IT leaders, care providers, and policymakers to take action. By improving EHR data tracking and expanding workforce education, “we can start to close the transgender care gaps and inform policy changes that improve accessibility and patient safety,” said Redman.
A copy of Redman’s HIMSS25 presentation can be found here.