 By Paula Braun
By Paula Braun
Twitter: @HHSIDEALab
It’s a familiar narrative. A crime drama opens with a dead body. Police are on the scene taking testimony from eyewitnesses, if there are any. A detective arrives and unravels the clues. How did this person die? More often than not, the answers aren’t obvious. That’s what makes it interesting.
In the world of public health, this drama unfolds every day, albeit in routine and often unglamorous ways. After a person is pronounced dead, a medical certifier must attest to the precise chain of events—diseases, injuries, or complications—that directly caused the death. Depending on the state, a medical certifier can be a physician, medical examiner, or coroner. This statement becomes part of the legal record that families use to settle the estate and governments use to issue or, more likely, stop benefits. Genealogists use the same records to map family trees. Law enforcement may use the records to help solve crimes. Mortality data serve multiple purposes and provide one of the best available sources to gain knowledge about health at the population level.
Throughout history, inquiries into causes of death have led to profound changes in cultural norms and practices to protect people and save lives. Ignaz Philipp Semmelweis discovered that hand-washing dramatically reduced the incidence of fatal puerperal fever. Florence Nightingale’s analyses revealed that typhoid and cholera killed more British soldiers than battle injuries in the Crimean war. More recently, E. Cuyler Hammond and Daniel Horn analyses of mortality data uncovered the link between smoking and the subsequent risk of death from lung cancer and other diseases.
Today, several acceptable ways of writing cause-of-death statements exist, yet the level of precision required can be daunting and confusing, especially when evidence is incomplete or there are multiple conditions present at the time of death. As an example scenario: An elderly female with senile dementia had been unstable on her feet. While walking, she fell and struck her head on the floor. She seemed to be okay, but was then found dead a few hours later on the sofa. Autopsy showed an occipital scalp hematoma and significant subdural hematoma.
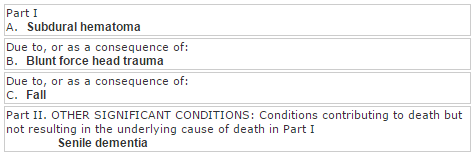
One approach to filling out the US Standard Death Certificate could be:
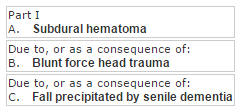 Another approach could be:
Another approach could be:
 This is a relatively straightforward example. However, if the decedent had multiple chronic conditions at the time of death, many of which presumably could have led to the fall, it becomes less clear which condition(s) to capture on the death certificate.
This is a relatively straightforward example. However, if the decedent had multiple chronic conditions at the time of death, many of which presumably could have led to the fall, it becomes less clear which condition(s) to capture on the death certificate.
Even in less complex examples, data accuracy may suffer when the certifier is not familiar with the medical or treatment history of the decedent. It’s also possible that key information may have been omitted to protect the reputation of the deceased or gratify the predilection of survivors.
Still, there is a need for timely, accurate, and actionable mortality data to inform public health interventions. In cases of vaccine-preventable deaths, such as those caused by the flu, it is incredibly valuable to know the precise strain to determine which interventions will most likely stop its spread. For other deaths, such as drug overdoses, it’s important to know the specific substances that were ingested. When these details are captured on death certificates, mortality data can greatly enhance existing public health surveillance efforts and help us understand epidemics.
Despite these difficulties, there are many ways to improve the accuracy of mortality data.
- Capture cause-of-death information electronically: Most states have electronic death registration systems. Entering data electronically eliminates difficulties in deciphering handwriting and minimizes the potential of inadvertent errors that may occur when handwritten data are keyed into a database. Electronic death registration systems also generally include data validation checks and additional guidance on how to complete a death certificate. These features are extremely helpful.
- Integrate death certificate training into physician board certification: It could be beneficial to include questions on physicians’ board certification tests about proper techniques for completing a death certificate and make proper certification a core competency for residency programs. The data captured on death certificates determine resource priorities. It’s important to get it right.
- Create interfaces between electronic medical records and other electronic sources, such as the National Violent Death Reporting System. As I highlighted in my last blog post, it is burdensome and frustrating to enter similar data both into electronic health records, as well as other public health surveillance systems. This leads to an inefficient and potentially error-prone data collection process. Some states have created cause-of-death modules that allow medical certifiers to enter data needed for the death certificate as part of their normal data entry process. These modules may help increase data accuracy, save physicians’ time, and save government registrars’ resources by not having to enter handwritten data into electronic databases.
- Develop clinical decision support tools to assist physicians in determining the sequence of events that most likely led to death. These tools could mine electronic health records to find patients’ diagnoses, medication history, laboratory results, progress notes, and other data to give medical certifiers a more complete picture of the trajectory of events that likely led to death. This could free physicians’ time to see more patients or spend more time with their patients.
- Recruit or serve as a data quality champion. It takes a village to complete a death certificate. Physicians, medical examiners, coroners, funeral home personnel, medical specialists, data entry clerks, and government registrars all play their respective parts. Do you have data collection or quality assurance expertise? Local champions could help lead trainings, answer questions, and help develop innovative solutions for improving data accuracy. They could also help track complicated cause-of-death cases that may take more time to resolve and are initially filed as pending.
About the Author: Paula Braun joined the IDEA Lab in November 2014, as part of the Entrepreneur-in-Residence (EIR) program at the U.S. Department of Health and Human Services (HHS). This article was originally published on HHS Idea Lab.
