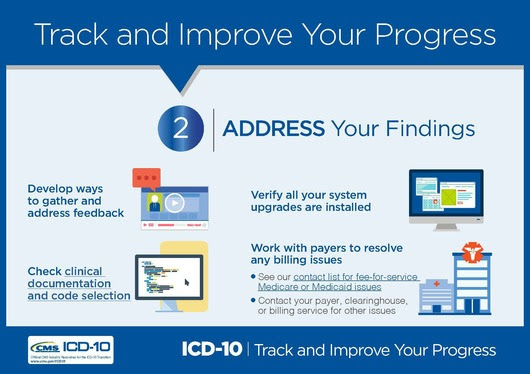
The Centers for Medicare & Medicaid Services (CMS) released a new infographic based on the Next Steps Toolkit to help you analyze your ICD-10 progress. By developing a feedback system, you can improve the accuracy of your clinical documentation and code selection, check for any systems issues, and resolve system problems with payers. Today, we will explore how to address your findings.
- Create processes to gather feedback and questions from your staff and to share insights throughout your organization.
- Create an issues list where staff can document new issues in one location as they arise. Track the system or payer with the issue, steps taken to resolve it, and the current status.
Check Clinical Documentation and Code Selection
- Look at clinical documentation for services provided before and after the October 1, 2015, transition date. Issues with documentation might result from insufficient clinician training on ICD-10 coding concepts and guidelines. Any lag times in responses to coder questions can further affect related key performance indicators (KPIs) such as days to final bill and rates of claims denied due to lack of medical necessity.
- Understand your organization’s processes for selecting diagnosis codes and applying coding guidelines to help identify the sources of issues and to target remediation efforts.
- Provide educational resources for your clinicians and coders.
- Identify a physician champion to act as a liaison and offer best practices.
Check for Systems Issues
- Verify that all of your systems have implemented available upgrades.
- Check for technical problems with your systems.
- Be sure your system is set to generate:
- ICD-10 codes and ICD-10 qualifiers for services provided on or after October 1, 2015.
- ICD-9 codes and ICD-9 qualifiers for services provided before October 1, 2015.
- Some providers who experience ICD-10 challenges because of system issues could benefit from contracting with a clearinghouse to process claims.
- Work with your vendor to resolve any systems issues affecting productivity.
Resolve Any Issues with Payers
- The Medicare/Medicaid Provider Contact List can be useful if you are experiencing issues with KPIs that are specific to Medicare Fee-For-Service (FFS) or Medicaid.
- For other issues with KPIs, contact your payer, clearinghouse, or billing service.
Keep Up to Date on ICD-10
Visit the CMS ICD-10 website and Roadto10.org for the latest news and official resources, including the Next Steps Toolkit, ICD-10 Quick Start Guide, and a contact list for provider Medicare and Medicaid questions. Sign up for CMS ICD-10 Email Updates and follow us on Twitter.