 An Example from the Emergency Department
An Example from the Emergency Department
By Jennie Welch, Vice President of Sales at Health Catalyst
This past March, my mother experienced symptoms that led our family to believe she might be experiencing a stroke. It was 7 p.m. on a Monday, and we headed straight for the Emergency Department (ED) of the best hospital in our area. My mother was discharged from the hospital at 1 a.m. the following morning with an order to follow-up with her regular doctor. It was interesting to watch the clinical workflow of the ED, and I reflected on some ways our experience may have been improved.
During this six-hour ordeal, I had a rare opportunity to view the hospital from the other end of the stethoscope. As a registered nurse who spent years in hospital EDs of all sizes across the country, I know the protocols and timeframes for ruling out or treating strokes. What we experienced from an outcomes perspective that night was positive, but during the long periods of time between medical tests and conversations with my mother’s care team, I observed many opportunities to improve the clinical workflow. Had my mother’s condition been more serious that evening, the workflow would have been critical to her ultimate outcome.
Efficient clinical workflow saves time, saves money, and saves lives. And in today’s industry, workflow can have a significant effect on reimbursement.
ED Workflow and Value-based Care Delivery
Workflow is defined as a process involving a series of tasks—how tasks are accomplished, in what order, and by whom. Clinical workflow simply refers to the delivery of clinical services.
The quality of care in the ED is especially dependent on efficient clinical workflow. Keep in mind that the Centers for Medicare and Medicaid Services (CMS) requires EDs to publicly report throughput metrics on:
- Median time of arrival to departure for admitted patients
- Median time from arrival to departure for discharged patients
- Median time from admit decision to departure for admitted patients
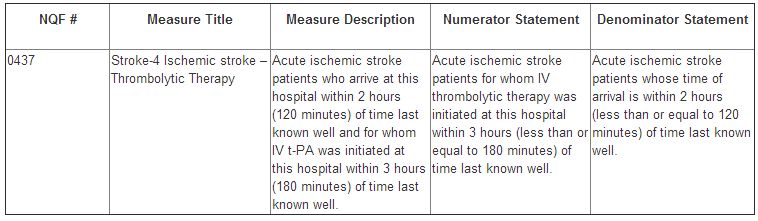
And by Q4 2014, these throughput metrics will affect reimbursement. In some cases—that of stroke, for example—efficient workflow and throughput are critical to clinical outcomes. That is why CMS will begin tying reimbursement to so many stroke measures. Here is just one example of these measures:
Throughput metrics are also important because they can affect patient satisfaction scores that are publicly reported and tied to reimbursement from CMS. When ED patients wait long periods of time to be treated, the percentage of patients who leave without being seen (LWBS) increases. This reduces volume and possible admissions and creates a potentially hazardous situation for those patients experiencing serious health issues.
Throughput also affects the volume of patients an ED can treat in a set period of time. If the average length of stay (LOS) for an ED with 20 beds is 4 hours, that ED can see 120 patients per day. The same ED with a LOS of 3 hours can see 160 patients. This extra soft capacity allows EDs to get patients into beds quicker, reducing the time for testing, and, in turn, speeding discharges. In my mother’s case, if a bed had been available when we arrived, it could have shaved two hours off of her stay.
My Mother’s Experience with ED Workflow
In my mother’s case, the clinical workflow highlighted the complicated and often inefficient use of everyone’s time in providing for her care and treatment. Keep in mind that this occurred at the highest-rated ED in the area.
As soon as we arrived at the ED, I took my mother to the point-of-care desk where a nursing assistant asked some preliminary questions, took her vitals, and added her to the computer. From a reimbursement perspective—and from the perspective of my mother’s health—the clock was now ticking.
Soon afterwards, a physician assistant came out to assess my mother and quickly ordered a CT scan, chest x-ray, lab work, and a urine test. He assigned her an ESI, or Emergency Severity Index, level 2 (1 being the highest acuity level; 5 being the lowest). We had a seat in the waiting room and waited a few minutes before the CT tech wheeled my mother off for her first and most important diagnostic test. A few minutes later she returned to the waiting room with the rest of our family and we waited for the triage nurse to finish up with a previous patient.
Once in triage, my mother and I carefully answered the questions about her previous history, signs and symptoms, medications, emotional state, abuse screen, and on and on. Unfortunately, the nurse was interrupted several times during triage with calls about other patients and visits from other nurses about other patients. Triage took half an hour instead of the usual 15 to 20 minutes. We then headed back to the waiting room where an x-ray technician was waiting to take my mother back for a chest x-ray. She returned and was given a specimen cup for a urine sample. It had been two hours since we arrived, and we were still waiting on a room.
Finally at about 10:00 p.m., three hours after arriving, we got a room. Within 15 minutes my mother was gowned, had an IV in place, blood drawn, and was hooked up for an EKG. The doctor came in later and said the CT was clear with no signs of a stroke. He was waiting for the lab work to come back to rule out any cardiac issues. The lab tests had to be prepped and processed and each test had a different processing time. Had the labs been drawn when my mother was having her CT scan and chest x-ray, the results would have been available by the time the physician entered the room.
Over an hour passed with no news. Finally, at 12:30 a.m., the doctor came in and said he had ruled out the most serious issues and that he was releasing her to see her regular doctor for more testing and follow-up. Around 30 minutes later, we got to go home.
How to Improve ED Workflow and Throughput
So what can be done to improve ED workflow? I have two suggestions to present here:
- Value-stream mapping
- Throughput analytics
Value-stream mapping
Value-stream maps are useful for pinpointing workflow process improvement potential. The concept of value-stream mapping is simple but highly effective: identify the flow of work throughout the ED for various conditions (e.g., stroke). Then evaluate the flow and determine the most effective method (the best practice) for carrying out each step in that process. By standardizing these best practices, you can eliminate waste in your processes.
Throughput analytics
It is hard to improve workflow without having a benchmark of where you started and a means to track the improvement that results from any changes you implement. Advanced analytics applications running on an enterprise data warehouse (EDW) platform enable EDs to track a variety of throughput measures and diagnose workflow bottlenecks.
By measuring each component of ED throughput—frontend flow (door to bed), middle flow (bed to disposition), and backend flow (disposition to discharge)—we can create strategies to remove the waste and inefficiency at each stage in the process. That’s better for anyone who finds themselves on either side of the healthcare system.
This article was originally published on Health Catalyst and is republished here with permission.
