 By Greg Kefer, Chief Marketing Officer, Lifelink Systems
By Greg Kefer, Chief Marketing Officer, Lifelink Systems
Twitter: @lifelnksystems
Every time we flip the calendars for the new year, there is no shortage of predictions from the various industry influencers and luminaries. The subject matter is frequently tech-focused and we often see the same themes repeated year after year. And, if you read enough of the predictions for the healthcare industry, one of the annual favorites is some version of this theme: “better interoperability.”
The definition for interoperability is about as clear as tech jargon can get:
In·ter·op·er·a·bil·i·ty (n)
The ability of computer systems or software to exchange and make use of information.
Who wouldn’t want to pull that off?
A Google search into “healthcare interoperability” brings more than 22 million URLs to click on. Conversely, it’s impossible to use Google to find data on exactly how much IT investment has been made to solve the interoperability problem. We know it’s a big challenge, but how big?
In light of the fact that system interoperability remains a top IT priority, consuming a chunk of massive healthcare IT budgets for most of the 21st century, it’s not unrealistic to assume the investments in system interoperability runs well into eight, maybe even nine figures.
Here’s the reality. Interoperability, no matter how people define it, may never be fully solved. Anything that is supported by 22 million sources of information on the internet has to be hard because most of that content is created by the vast commercial ecosystems that arise when billions of dollars start flowing in to solve a big IT problem.
Will Companies Ever Achieve the Single Version of the Truth Vision?
Huge, sustained investments will deliver results. Maybe newer, smaller companies that don’t face extensive legacy IT debt can get there. And many IT leaders will declare this problem has been solved at their organizations. The reality is that interoperability projects never end because data and systems are fundamentally pretty rigid animals.
Mergers and acquisitions can bring more disconnected IT into an organization. Software upgrades and code changes are happening all the time. And technology must constantly evolve to keep pace. It’s never static. Every change, even the slightest, has the potential to break a connection or process.
I spent a decade working with IT executives from 60 of the world’s biggest companies trying to improve interoperability between their supply chain systems and those of their major logistics partners that they all used to move ocean freight. We called it the global shipper council. The charter was to leverage the collective power of multiple huge companies to drive standards so the entire industry would benefit.
The shipper council focused on just seven logistics events across the top 20 trade lanes. Data quality would ebb and flow constantly. We had dozens of project managers and engineers focused on it 24 hours a day. In short, it was a never-ending battle that ultimately had to be an ongoing part of any digital supply chain program.
In healthcare, the combination of ongoing M&A, stiff compliance regulations, and complexity makes IT hard, expensive, and slow. But the pressure to improve is only increasing. Rising costs, tight labor, and the need to digitally engage patients puts a premium on all things digital.
There are Lots of Smartphones Out There
The digital patient engagement opportunity will be crucial in the next decade. The baby boomer generation is retiring and shifting into Medicare. According to Pew Research, 10,000 men and women retire each day and that is expected to double Medicare and Medicaid costs. At the same time, the COVID-19 pandemic has triggered a massive labor shortage that shows no signs of slowing down. It’s a perfect storm.
The path forward is digital, and with smartphone penetration approaching 90%, any patient-facing technology must be mobile.
But so far, the industry has failed to drive sustained engagement with the vast majority of patient populations. A recent study found that just 7% of consumers use mobile apps from their healthcare providers on a regular basis. This is a huge problem.
The key problem with mobile apps is that there are too many of them and they are too hard for most patients to use. A patient might need to use four different apps as part of a treatment program for a broken bone — one from the hospital, one from the orthopedic specialist, one from the pharmacy, and one from the physical therapist. Each requires its own download, username, password. And each app looks like it came from a different planet.
There will likely never be that super, all-encompassing mobile app covering every aspect of patient care. There are too many stakeholders, there is too much institutional resistance, and the regulatory/privacy hurdles are extreme. Maybe Apple or Amazon will figure it out, but if that happens, the industry incumbents will find themselves in a different kind of battle — something more along the lines of staying in business.
Mobile technology has evolved and is moving beyond apps. Conversational AI can run on a mobile device outside of the commercial app domain. Using smart messaging, patients interact with chatbots to handle all aspects of healthcare. There are a number of compelling use cases that show high engagement and satisfaction with conversational AI, but it’s still early.
Conversational AI Needs Personalization which Interoperability Makes Possible
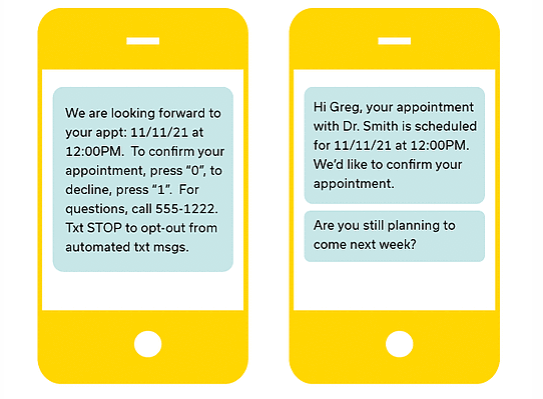
Creating a level of interoperability between the systems that hold all of the patient information and the conversational AI solution is vital. The difference between “Hi Greg” and “Press 0” may be subtle, but it is a significant component to driving the desired outcome — getting a patient to successfully complete a task on their mobile device, and doing it with a high degree of satisfaction.
From an interoperability perspective, the data required to pull off a pre-appointment check-in could reside in several systems of record. A CRM system may hold all of the patient contact information, while an EMR system may hold relevant clinical information. With a conversational layer sitting on top of, and across the various systems, the integrations are actually somewhat manageable.
One of the most important aspects of engagement is personalization. A smart chatbot should know the name of the patient’s doctor, and the date of the last appointment, and the prescription history — all data that resides in back office systems of record.
Consider these two experiences and it’s not hard to understand which one is more effective:
The data “plumbing” between different systems is getting easier and the costs are going down. The advent of APIs has created an entire technology market, where vendors such as Redox are providing out-of-the-box connectivity specialized for healthcare. Connecting data pipes alone does not suddenly activate an army of super smart digital assistants, but it is a step in the right direction.
There are headwinds and lots of opinions about a big topic like interoperability. It’s complex for a reason. But rather than waiting for the day when single-version-of-truth-status inside the enterprise has been achieved (which may be never), the need to drive massive digital engagement scale between providers and patients has arrived.
The path forward will be virtual. It’s either a windy dirt road, or an eight-lane super highway. Patients prefer the latter.
This article was originally published on LifeLink Systems and is republished here with permission.
