 By Judah Thornewill, Bob Esterhay, M.D., Eric C. Schneider, M.D., Aneesh Chopra and William Yasnoff, The Commonwealth Fund
By Judah Thornewill, Bob Esterhay, M.D., Eric C. Schneider, M.D., Aneesh Chopra and William Yasnoff, The Commonwealth Fund
Twitter: @commonwealthfnd
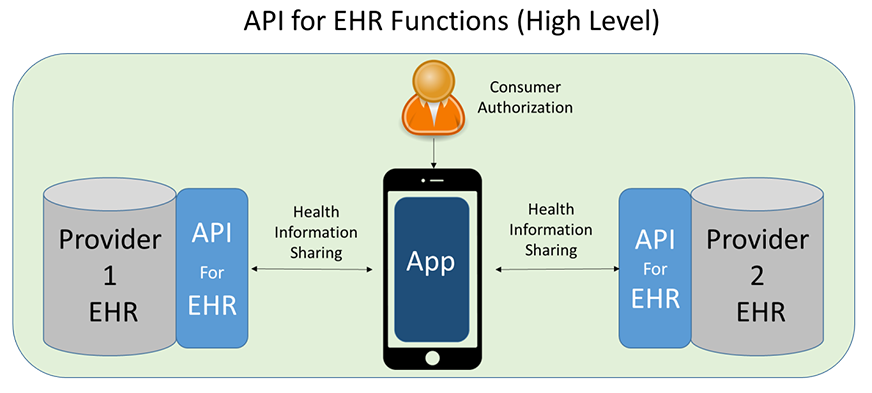
While more and more doctors’ offices, hospitals, and other providers are using electronic health records (EHRs), patients rarely have access to their digital health data. And patients need more than access. They need to be able to view and share their data readily and rapidly. Picture a mobile phone app that updates a patient’s doctors and pharmacy whenever a prescription is changed, or that allows test results from a specialist’s office in one city to be shared with a primary care physician back home.
Making digital health data useful to patients is a national priority—and application program interface technologies, or APIs, are needed to realize this goal. API technologies, adopted widely in banking and retail, make it possible to move information easily between computer systems or programs. APIs are used to let ATMs connect to banks and airline systems to connect to travel portals.
APIs have the potential to remove many barriers to the sharing of health information between providers, patients, and others but they are fairly new to health care. In addition, not all types of APIs are equal when it comes to sharing digital health information. Some restrictive APIs could even be used instead to block patients from accessing their health information.
APIs are starting to enter the EHR market because of the U.S. government’s Health IT Certification Program authorized under three federal laws: the Health Information Technology for Economic and Clinical Health (HITECH) Act, the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), and if it’s signed by President Obama as expected, the 21st Century Cures Act. The certification program incentivizes the exchange of interoperable information between EHRs and other health IT systems such as apps, pharmacy systems, or laboratories. APIs for EHRs must include features such as identity authentication and must enable secure exchange of digital health data in a form that can be read and used by other computers the way a shopping order from one computer can be verified by another. Because there are a variety of distinct EHRs and other health data systems that must communicate to mobilize health data, APIs are key to advancing health record interoperability.
Having openly accessible APIs could provide consumers (and other trusted entities they designate) with unrestricted, no-cost access to their own personal digital health information, thereby empowering better health, better care, and smarter spending. Benefits include:
- strengthening consumers’ ability to get, use, and share health information
- making it easier for them to move among providers
- helping providers coordinate care across settings
- reducing entry barriers and promoting innovation for new health apps, devices, and services.
Several actions could be taken to encourage broad adoption of openly accessible APIs. In the public sector:
- Congress has encouraged the use of openly accessible APIs for patient health data through the recently enacted 21st Century Cures legislation.
- The Department of Health and Human Services (HHS) could use its authorities under previous legislation (HITECH and MACRA) and through 21st Century Cures to update its Health IT Certification Program to include consumer access to openly accessible APIs.
- HHS and/or Congress could fund development of open-source, standards-based API for EHR technologies through standards development organizations or groups of industry representatives.
In the private sector, actions to encourage open APIs include:
- Encourage public commitments from leading providers, payers, and EHR vendors to use openly accessible APIs through “consumer empowerment and interoperability pledges” or other public declarations.
- Provide purchasing tools such as model contracts and purchasing guides to help health providers procure openly accessible APIs.
- Invest in continued development of open-source API technologies through industry groups such as standards development organizations or market-driven consortia.
- Investment in open-source technologies should lower the cost of entry for new market entrants seeking to sell APIs to EHR vendors and providers. Providers and EHR vendors should support the ability to choose among multiple openly accessible APIs to encourage competitive markets for openly accessible APIs.
- Develop consensus standards for openly accessible APIs and related technologies.
If policymakers, delivery system leaders, and consumer advocates encourage the use of open APIs in health care now, they will clear a path for innovative uses of electronic health data that serve the needs of patients, thereby improving the quality and affordability of health care.
This article was originally published on The Commonwealth Fund Blog.
