 By Kimberly Brandt, Principal Deputy Administrator for Operations, CMS
By Kimberly Brandt, Principal Deputy Administrator for Operations, CMS
Twitter: @CMSGov
The Centers for Medicare & Medicaid Services (CMS) is committed to reducing improper payments in all of its programs, as evidenced by improper payment reduction efforts contained in the Fiscal Year 2018 President’s Budget. CMS’s new leadership is re-examining existing corrective actions and exploring new and innovative approaches to reducing improper payments, while minimizing burden for its partners. Due to the successes of actions we’ve put into place to reduce improper payments, the Medicare Fee-For-Service (FFS) improper payment rate decreased from 11.0 percent in 2016 to 9.5 percent in 2017, representing a $4.9 billion decrease in estimated improper payments. The 2017 Medicare FFS estimated improper payment rate represents claims incorrectly paid between July 1, 2015 and June 30, 2016. This is the first time since 2013 that the Medicare FFS improper payment rate is below the 10 percent threshold for compliance established in the Improper Payments Elimination and Recovery Act of 2010.
Improper payments are not always indicative of fraud, nor do they necessarily represent expenses that should not have occurred. For example, instances where there is insufficient or no documentation to support the payment as proper are cited as improper payments under current Office of Management and Budget guidance. The majority of Medicare FFS improper payments are due to documentation errors where CMS could not determine whether the billed items or services were actually provided, were billed at the appropriate level, and/or were medically necessary. A smaller proportion of Medicare FFS improper payments are payments for claims CMS determined should not have been made or should have been made in a different amount, representing a known monetary loss to the program.
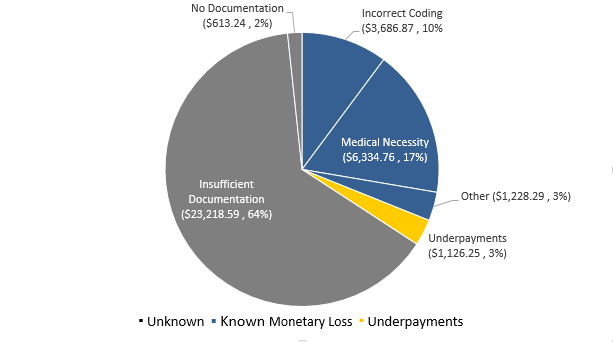
Figure 1 provides information on Medicare FFS improper payments that are a known “monetary loss” to the program (i.e. medical necessity, incorrect coding, and other errors). The estimated known “monetary loss” improper payment rate is 3.0 percent, representing an estimated known monetary loss of $11.3 billion out of the total estimated improper payments of $36.2 billion. In the figure, “unknown” represents payments where there was no or insufficient documentation to support the payment as proper or a known monetary loss. In other words, when payments lack the appropriate supporting documentation, their validity cannot be determined. These are payments where more documentation is needed to determine if the claims were payable or if they should be considered monetary losses to the program.
Figure 1: FY 2017 Medicare FFS Improper Payments (in Millions) and Percentage of Improper Payments by Monetary Loss and Type of Error
CMS continues to implement tools and work with law enforcement partners and other key stakeholders to help focus on prevention, early detection, and data sharing to prevent and reduce improper payments in Medicare FFS. Although documentation errors are the largest cause of improper payments, CMS employs multi-layered efforts to target all root causes of improper payments, with an emphasis on prevention-oriented activities.
CMS is pleased to have achieved this reduction in the improper payment rate, but we still have work to do. We remain committed to collaborating across CMS and with stakeholders to address potential vulnerabilities and continuing to strengthen our program integrity efforts, while minimizing burden for our partners.
This article was originally published on The CMS Blog and is republished here with permission.
