 By Anshu Jindal, COO, MyMipsScore
By Anshu Jindal, COO, MyMipsScore
Twitter: @MyMipsScore
Recently Medicare Part-B providers got their much awaited MIPS eligibility status letters from CMS. If you got MIPS exempt status as individuals (NPI level), pay close attention. Before making the decision to report or not to report, you need to understand what does reporting for MIPS mean and how it impacts you. The impact of reporting (or not reporting) for MIPS is two-fold: Financial and Reputational.
MIPS Reporting – Financial Impact
It is very important to understand that if you are included in MIPS, you are required to report and will receive a payment adjustment (positive or negative) based on your performance on the data you report.
- Positive payment adjustment is not a fixed bonus that you can earn. It is variable and will apply as a percentage of your Medicare Part-B billing charges. The percentage of positive payment adjustment will be determined by your MIPS score and that of your peers. There is additional Exceptional Performance Payment Adjustment (up-to 10%) if your MIPS score is more than 70.
- Negative payment adjustment is not a fixed penalty either. This is variable too and will also apply as a percentage of your Medicare Part-B billing charges. CMS has made it very easy for 2017 (transition year) to avoid penalty and stay in the neutral zone with Pick-Your-Pace options. Don’t overlook the impact of score on your reputation though.
MIPS Reporting – Reputation Impact
Score for all the clinicians who report for MIPS would be made publicly available on Physician Compare website. Provider performance on certain quality measures would also be public just like for PQRS. If you choose not to report, you will not be listed on the physician compare site. There would be no score for you. Is that okay with you/your practice?
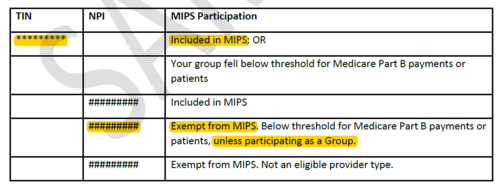
Interpreting the MIPS Eligibility Letter
Now that we have some understanding of the impact of reporting/not reporting, let’s see what your eligibility letter means for you and your group if your group TIN is included in MIPS, but you are exempt from MIPS at the NPI level with help of two examples.
1. A Group of 80 Providers, Where Only 1 Provider is MIPS Eligible as an Individual, While 79 Providers Are Not.
This group has two reporting options:
Option-A: Only one eligible provider reports as an individual, while rest of the providers don’t
- Medicare payment adjustment will apply to only one provider who reports. Rest of the providers don’t get any payment adjustment. Your practice could be missing a huge earning opportunity. Let’s assume that the group’s Medicare Part-B billings are $1,500,000 (very modest number for an 80 provider group), but the eligible provider’s billing is only $30,000. Let’s play a little with numbers to see the impact of payment adjustment for group reporting vs. individual reporting for this group.
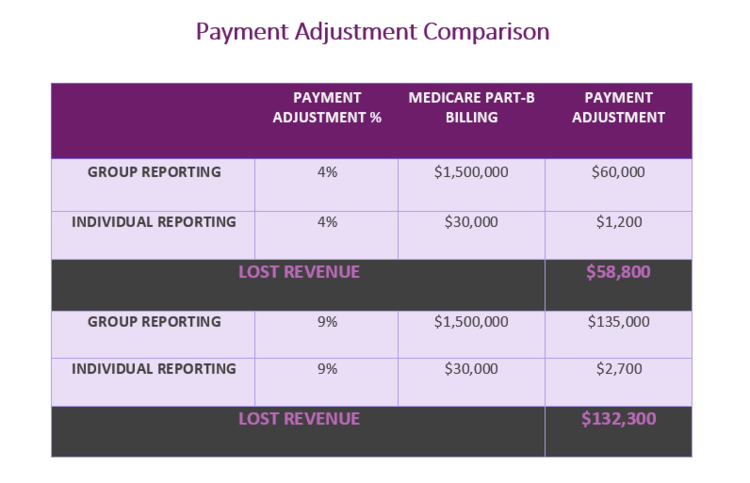 The numbers speak for themselves. Not reporting as a group will have huge negative financial impact. The group takes a $58,800 hit at just 4% bonus. If you are an excellent team and can earn 9% bonus by working together, you would potentially lose $132,300 by not reporting as a group. So the big question is: What are you saving by not reporting as a group? Mind you, we are not taking into account the reputation here. Just the money.
The numbers speak for themselves. Not reporting as a group will have huge negative financial impact. The group takes a $58,800 hit at just 4% bonus. If you are an excellent team and can earn 9% bonus by working together, you would potentially lose $132,300 by not reporting as a group. So the big question is: What are you saving by not reporting as a group? Mind you, we are not taking into account the reputation here. Just the money.
- Only the clinician reporting will have a MIPS Score on Physician Compare website. Rest of the providers don’t get any score. That will hurt in short term and long term. It will hurt both the reputation and finances of the group and the clinicians. If ever non reporting clinicians want to move to a different state or change groups, not having a score will significantly reduce their bargaining power.
- Group will be unprepared when the requirements get stringent from 2018 on-wards, and might incur negative payment adjustment and thus a significant financial hit.
Option-B: All the providers report collectively as a group under one TIN
- All providers get the same payment adjustment based on the group score. Numbers quickly add up.
- All providers get a MIPS Score that will stay with them in case they change groups.
- All providers and the group will be all set for higher thresholds, tougher requirements of MIPS in upcoming years.
2. A Group of 5 Providers Who Meet the Volume Threshold Requirement at the TIN Level, But None of Them Have Sufficient Volume to Qualify at the NPI Level.
This group has two choices too: (A) Report as a group (B) Not report at all . The pros and cons of reporting and not reporting are same as that of the larger group.
The decision to move from reporting as a group to reporting as an individual or vice versa and should not be taken lightly. MyMipsScore’s provider level analysis makes this really simple for you. You can compare the scores of every provider reporting individually with the group score (all providers combined). You can also find out the best measures that work for you as a group.
Ultimately the choice is yours. You can push the easy button this year. Sit back. Relax. Enjoy the MIPS exempt status. Or you can utilize this great opportunity to report under MIPS to build a name for your practice and earn incentives.
Contact us today to learn more and make decisions based on facts.
This article was originally published on MyMipsScore and is republished here with permission.
