By Anshu Jindal, COO, MyMipsScore
By Anshu Jindal, COO, MyMipsScore
Twitter: @MyMipsScore
The onset of MACRA in 2017 marks the big shift to value-based-care. It is a big and bold step towards providing best possible quality at the lowest possible cost. An initiative of such proportion inherently has a lot of moving parts. 2017 being the first year of implementation of Quality Payment Program (QPP), CMS is still working out the kinks, seeking feedback, and making clarifications available as the issues come up. Still, there are a lot of information gaps to be filled, misinformation removed, and confusion dispelled.
Caveat Emptor – Cost & Quality of FREE Advice
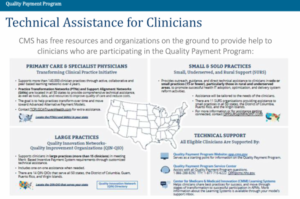
CMS has brought multiple organizations on board to help educate the healthcare organizations and providers about different aspects (MIPS, APMs, Advanced APMs) of Quality Payment Program (QPP). These organizations operate under four different heads:
- Transforming Clinical Practice Initiative (TCPI) – For primary care and specialist physicians
- Small Underserved and Rural Support (QPP-SURS) – For small (solo, groups of 15 or less), underserved, and rural practices
- Quality Innovation Networks – Quality Improvement Organizations (QIN-QIO) – For large practices of 15 or more clinicians
- Technical Support – To everyone connected with MIPS/APMs in any way
CMS has earmarked 100 million dollars for 2017 – 2021 (20 million dollars per year) to be given to the eleven organizations under the newest initiative (QPP-SURS) to provide education, clarification, and MIPS assistance to the group with least resources- the small and under-served rural practices.
All these organizations are putting out educational content in multiple shapes and forms. The effort is well meaning. However, there is some inaccurate information floating around. What’s dangerous is that this incorrect information is sandwiched between mostly correct information. How is one to know? Anyone would trust the information completely as it comes from a source funded by CMS. Such misinformation, or partially correct advice has potential to do more harm than good. With so much at stake for the providers, we can’t afford to lose critical decision making nuances in the static of misinformation and knowledge gaps.
This raises the question of accountability. The names of these organizations are all over the CMS information materials and this press release. But, nowhere does it mention how their performance would be measured, and how will they get paid. Nor is there any mention of any consequences for disseminating incorrect information or for giving bad advice. Shouldn’t there be one? This so called FREE advice isn’t free either. Our tax dollars fund it. So don’t we have the right to know?
Is Pick-Your-Pace a Worthy Choice?
On one hand providers are offered a Pick-Your-Pace option in 2017 by CMS. On the other hand, their scores will be published on the CMS Physicians Compare website and most likely syndicated on other public sites like Health Grades. Providers are given the option in 2017 to avoid 2019 negative payment adjustment with minimal effort. That’s good, but they have to read the fine print to know that their score on a 0-100 point scale will be 3 and made public. It’s just like saying, we will wave off the fine on this speeding ticket, but it will still show in your driving history, and will impact everything related to it. Only difference being that MIPS score is going to have more profound impact on a provider’s career in the value-based world – negotiating contracts with insurance companies, changing jobs, selling a practice just to name a few in addition to impact on reputation. Any advice to use this option should be followed by a giant asterisk to bring attention to the downside of this choice.
Physician Report Cards – Why now?
No one likes report cards, including healthcare providers, and the recent MGMA poll proves it. Given the diversity of the healthcare providers, their specialties, their challenges, and the kind of care that they provide, it is a gargantuan task to create a single report card that will feel fair to all from the get go. Just like any other report card, it will miss some points, and will be a bit unfair to some. But we got to start somewhere. No matter which industry we pick, the compensation is tied in some form to a metric. It’s finally coming to healthcare too in the form of Value-Based-Reimbursement and it’s here to stay. No point sitting and complaining. We better get ready for it.
We can’t improve what we can’t measure, and we definitely can’t progress if we can’t improve.
This article was originally published on MyMipsScore and is republished here with permission.