 By Lucy Zielinski, Managing Partner, Lumina Health Partners
By Lucy Zielinski, Managing Partner, Lumina Health Partners
Twitter: @LuminaHP
The new CMS 2021 Physician Fee Schedule (PFS) went into effect on January 1, 2021. Most of the final rule consists of expected policy refinements, but the regulations do include some significant changes that will impact medical practice productivity, strategy and revenue.
To take full advantage of the new fee schedule, physicians and medical practice leaders should focus on three immediate priorities:
1. Evaluate How the New Conversion Factor Will Impact Revenue
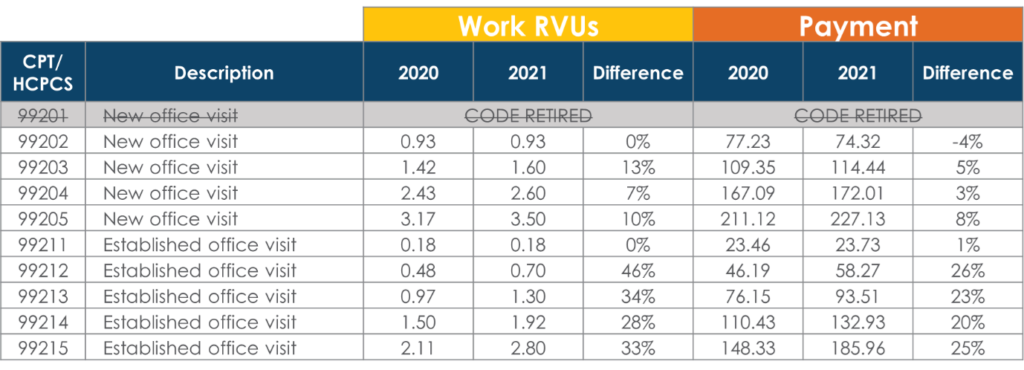
The new PFS has cut the payment conversion factor from $36.09 to $34.89, a decrease of more than 3%. However, CMS has also increased relative value units (RVUs) for several evaluation and management (E/M) codes. For example, the most utilized code for established patients is 99213. Under the new fee schedule, work RVUs for this code have increased by 34% and payment has increased by approximately 23%.
Here is a snapshot of some important E/M code changes and what they mean for physician payment:
How will these changes affect practice revenue? It all depends on your practice’s service mix, service utilization and payer contracts. To assess the revenue impact for your practice:
- Identify your practice’s 2020 unit volume by CPT code
- Use the 2020 PFS to establish your baseline revenue
- Run the same calculation using 2021 work RVUs and the updated conversion factor
To help with this analysis, Lumina has created a 2021 PFS Impact Calculator that simplifies the process. Once you have determined how the new PFS will affect gross practice revenue, calculate the impact on operating margin. Depending on what you find, you may need to explore new options for managing the bottom line:
Identify opportunities to reduce expenses: Now that a large percentage of visits have been converted to telehealth, many practices are in a position to reassess their facility needs and streamline their real estate costs. In addition, groups with employed physicians should analyze the new fee schedule’s impact on payroll. If your compensation model is based on work RVUs, physician pay could increase up to 25% or more. One approach: Maintain 2020 work RVUs in your 2021 compensation model and then re-balance the plan at the end of the year.
Identify opportunities to increase revenue: Begin by assessing your practice’s charge lag, first-pass clean claim rate and overall denial rate. Identify any shortfalls against national benchmarks and implement process changes to improve performance. Practice leaders should also analyze their payer contracts. There are currently many opportunities to negotiate higher incentive payments for value-based agreements. In addition, if your practice participates in the Merit-Based Incentive Payment System (MIPS), determine what you need to do to earn “exceptional performer” bonuses.
2.Take Advantage of Relaxed Requirements for E/M Visits
In addition to increasing payment for many E/M codes, CMS has also relaxed documentation requirements for these visits.
Previously, physicians were required to document office visits based on patient history, physical exam and medical decision-making (MDM). For visits dominated (more than 50%) by counseling and/or coordination of care, documents could be based on time.
Starting in 2021, history and physical documentation has been eliminated for code selection purposes. Physicians can now document E/M codes based on either MDM or time:
Documenting based on MDM: The new medical decision-making table from the American Medical Association spells out simplified requirements for determining service level.
Documenting based on time: The “more than 50%” requirement no longer applies. Simply document the total time (including face-to-face and non-face-to-face time) that the physician personally spends before, during and after the visit on the date of the visit.
The goal of all these changes is to reduce administrative burden by simplifying code selection so it is more clinically relevant and intuitive.
What should practice leaders do to take advantage of these changes? First, work with IT staff to revise your electronic health record (EHR) templates to reflect the new regulations. Second, educate physicians on the new simplified requirements. This is a significant opportunity for physicians to reduce clinically irrelevant documentation and truly put patients over paperwork.
3. Build Your Practice’s Telehealth Capabilities
As everyone knows, telehealth utilization exploded during COVID-19. Before the pandemic, only about 15,000 Medicare fee-for-service beneficiaries received a telemedicine service in any given week. During the height of the pandemic, that weekly average increased to more than 800,000.
The 2021 PFS reflects this new reality. The list of covered telehealth services now includes nearly 250 codes, including codes for home visits and psychological and neuropsychological testing. (See the current List of Telehealth Services payable by Medicare.) Note that about 35% of these covered codes allow for audio-only services.
Overall, the new rule is a strong signal that telehealth is here to stay and will only grow as a revenue opportunity for medical practices. Right now, physicians and practice leaders should examine ways to expand their telehealth program:
New telehealth services. If your practice has been using telehealth mainly to manage patients with existing problems, consider expanding your program to services such as annual wellness visits, depression screening and counseling/coordination of care. You can also use telehealth to review test results with patients and manage their prescriptions.
Chronic care check-ins. Telehealth provides the opportunity to meet more frequently with chronic care patients. Consider enhancing your virtual chronic care check-ins by incorporating physical therapists, occupational therapists and/or licensed clinical social workers into the process.
Remote monitoring services. Medical practices should also consider partnering with a home health agency to provide remote monitoring for homebound patients. This is a strong opportunity to improve your care of older patients while building practice revenue.
In addition to expanding your telehealth services, work on refining your execution. Most practices can improve all their remote services by improving the telehealth experience for patients. Use pre-visit planning to ensure a smooth workflow. In addition, look for ways to use more video during visits and consider investing in better video equipment. Higher physician visibility equals higher patient satisfaction and a more successful telehealth program.
More Practical Strategies
The 2021 Physician Fee Schedule contains important opportunities to increase practice revenue, simplify provider documentation and improve patient care.
This article was originally published on the Lumina Health Partners blog and is republished here with permission.
