 According to new data published by the AAMC (Association of American Medical Colleges) (@AAMCtoday), the United States could see an estimated shortage of between 54,100 and 139,000 physicians, including shortfalls in both primary and specialty care, by 2033.
According to new data published by the AAMC (Association of American Medical Colleges) (@AAMCtoday), the United States could see an estimated shortage of between 54,100 and 139,000 physicians, including shortfalls in both primary and specialty care, by 2033.
“This annual analysis continues to show that our country will face a significant shortage of physicians in the coming years,” said AAMC President and CEO David J. Skorton, MD. “The gap between the country’s increasing health care demands and the supply of doctors to adequately respond has become more evident as we continue to combat the COVID-19 pandemic. The challenge of having enough doctors to serve our communities will get even worse as the nation’s population continues to grow and age.”
The sixth annual study, The Complexities of Physician Supply and Demand: Projections from 2018-2033, was conducted prior to the rise of COVID-19 for the AAMC by the Life Science division of IHS Markit, a global information company. This analysis, conducted in 2019, includes supply and demand scenarios and was updated with the latest information on trends in health care delivery and the state of the health care workforce, such as data on physician work hours and retirement trends.
Projected Physician Shortages by 2033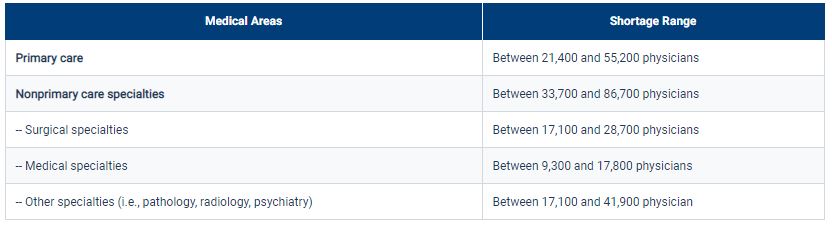
“As our health care system continues to treat patients during the COVID-19 pandemic, the need for a strong and sufficient health care workforce is more apparent than ever. Specialty physician shortages, especially those that are hospital-based, including critical care, emergency medicine, and pulmonary specialists, are particularly urgent,” Skorton said, noting that hospitals in hard-hit areas have had to rely on a patchwork of solutions, including expanding scope of practice laws, graduating students early from medical schools, hiring physicians out of retirement, and relocating physicians from other geographic regions to staff their inpatient units.
Other key findings from the report include:
- Demographics — specifically, population growth and aging — continue to be the primary driver of increasing demand from 2018 to 2033. During this period, the U.S. population is projected to grow by 10.4% from about 327 million to 361 million. The U.S. population under age 18 is projected to grow by 3.9%, while the population aged 65 and over is projected to grow by 45.1% by 2033. Therefore, demand for physician specialties that predominantly care for older Americans will continue to increase.
- A large portion of the physician workforce is nearing traditional retirement age, and supply projections are sensitive to workforce decisions of older physicians. More than 2 of 5 five currently active physicians will be 65 or older within the next decade. Shifts in retirement patterns over that time could have large implications for the supply of physicians to meet health care demands. Also, growing concerns about physician burnout suggest physicians will be more likely to accelerate than delay retirement.
- If underserved populations were to experience the same health care use patterns as populations with fewer barriers to access, current demand could rise by an additional 74,100 to 145,500 physicians. This analysis underscores the systematic differences in annual use of health care services by insured and uninsured individuals, individuals in urban and rural locations, and individuals of differing races and ethnicities. These estimates, which are separate from the shortage-projection ranges, help illuminate the magnitude of current barriers to care and provide an additional reference point when gauging the adequacy of physician workforce supply.
Prior to the COVID-19 pandemic, physician shortages were already being felt by Americans nationwide. According to public opinion research conducted in September 2019 by Public Opinion Strategies for the AAMC, 35% of voters said they had trouble finding a doctor in the past two or three years. This is a 10-point jump from when the question was asked in 2015.
To help address the physician shortage, the bipartisan Resident Physician Shortage Reduction Act of 2019 (S. 348, H.R. 1763) was introduced in the U.S. Congress to provide increased Medicare support for an additional 3,000 new residency positions each year over the next five years.
“The pandemic has shown the importance of investing in a strong health care infrastructure. To ensure access to care, one essential step Congress must take is to ensure an adequate physician workforce by ending the freeze on federal funding for graduate medical education that has been in place since 1997 that limits federal support for training new physicians,” Skorton said. “In addition, our partners in health care, especially nurse practitioners and physician assistants, also have critical roles to play in what must be a multipronged solution to increase access to care and ensure our nation is prepared to adequately respond to public health needs and emergencies in the future.”
