 By Erica Galvez / Interoperability and Exchange Portfolio Manager, ONC
By Erica Galvez / Interoperability and Exchange Portfolio Manager, ONC
When individuals arrive at a hospital, whether on their own accord or in an ambulance during an emergency, the availability of key clinical information—such as current medications, test results or medication allergies—can help the attending care team provide safe, high quality care. This information often resides in health records across multiple provider settings. Lacking access to this information may put a patient’s health and wellness at risk.
How can we improve the availability of information at the point of care in hospital settings? Interoperable electronic health records (EHRs) have the capability to support electronic sharing of information between health care providers, which increases the availability of information at the point of care.
Recent ONC analyses from a nationwide survey of non-federal acute care hospitals conducted by the American Hospital Association (AHA) highlight the near universal adoption of EHRs by hospitals and significant increases in hospitals’ electronically exchanging health information with outside providers compared to past years.
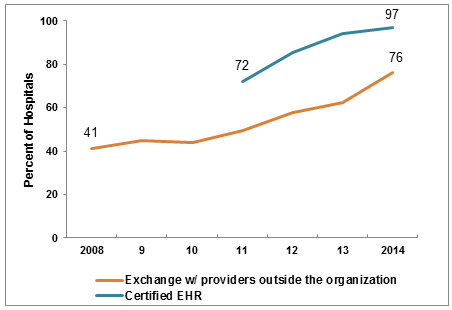
- Nearly all reported hospitals (97%) possessed a certified EHR technology in 2014, increasing by 35% since 2011.
- In 2014, three-quarters of hospitals reported that they electronically exchanged health information with outside ambulatory providers or hospitals. This represents a 23 percent increase since 2013 and an 85 percent increase since 2008, the year AHA started collecting this information.
Hospitals now have the infrastructure in place to electronically exchange health information and a majority of hospitals are sharing information with hospitals and ambulatory care providers outside their hospital system.
So to what extent do hospitals have the necessary clinical information at the point-of care?
In 2014, Some Hospitals Have Necessary Clinical Information at the Point-of-Care
A snapshot of the availability of clinical information among America’s hospitals shows that 41 percent routinely are able to access important health information about a patient during treatment from sources outside their hospital according to recent ONC analysis of 2014 data from the AHA.
This baseline estimate suggests that there is room for improvement. To that end, ONC is leading the charge on developing a Nationwide Interoperability Roadmap. In the near-term, the Roadmap focuses on enabling a majority of individuals and providers across the care continuum to send, receive, find and use a common set of clinical information by the end of 2017. These four basic exchange functions coupled with standardized clinical information that can be integrated into EHRs supports a variety of use cases and offers significant benefit to patients, care givers, and clinicians.
As seen in analysis of AHA data, there are concrete benefits to engaging in all of these activities for hospitals: greater availability of information at the point of care. Of the one-quarter of U.S. hospitals that are able to send, receive, find and use electronic health data, 86 percent reported that they are able to access important health data about a patient during treatment from sources outside their hospital. This is over twice the national average.
Why aren’t hospitals engaging in greater interoperable exchange?
Barriers to Exchange Exist
ONC Data Brief 25: Interoperability among U.S. Non-federal Acute Care Hospitals also highlights technical, operational and financial barriers which may be preventing greater interoperability. For example, only 4 in 10 hospitals reported they can integrate information from patient summary of care records into their EHRs, which poses challenges to clinical workflow and information usability. Exchange partners’ limited capability to receive information was considered by hospitals to be the top barrier. Long-term care and behavioral health care providers, in particular, have limited capabilities to electronically exchange data with outside providers. Other technical barriers relate to provider directories and patient matching, key priorities that the Roadmap seeks to address.
Looking Ahead
The results highlighted in this data brief illustrate that while most hospitals have EHRs and are actively exchanging health information electronically, important work remains to ensure that the necessary clinical information is available at the point of care in hospital settings. ONC will continue reporting on interoperable exchange among hospitals to understand where the nation is making progress, and identify where gaps and barriers remain. This will help inform the evolution of the Roadmap to craft policies and strategies to improve interoperable exchange.
This post was originally published on the Health IT Buzz and is syndicated here with permission.
