 By Tyler Williams, Partner, Payor Logic
By Tyler Williams, Partner, Payor Logic
Twitter: @PayorLogic
An impending Medicare card change will present new billing and reimbursement challenges for all healthcare providers—not just emergency medicine.
Beginning April 1, 2018, CMS is removing social security numbers (SSNs) from the Health Insurance Claim Number (HICN) of over 150 million Medicare recipients, including approximately 60 million active Medicare patients. The new Medicare Beneficiary Identifiers (MBIs) will be assigned over an 18-month crossover period with new Medicare cards sent directly to enrollees.
The main reason CMS is removing SSNs from the new Medicare cards is to fight medical identity theft. The goal is to better protect private health care, financial information, and federal health benefit payments. While the change will impact all providers, emergency services providers are expected to be particularly susceptible to billing errors and reimbursement delays since most of their patients are one-time encounters without established relationships.
Here is what you need to know about the timeline, transition, exceptions, and how to prepare.
Timeline for the new Medicare cards
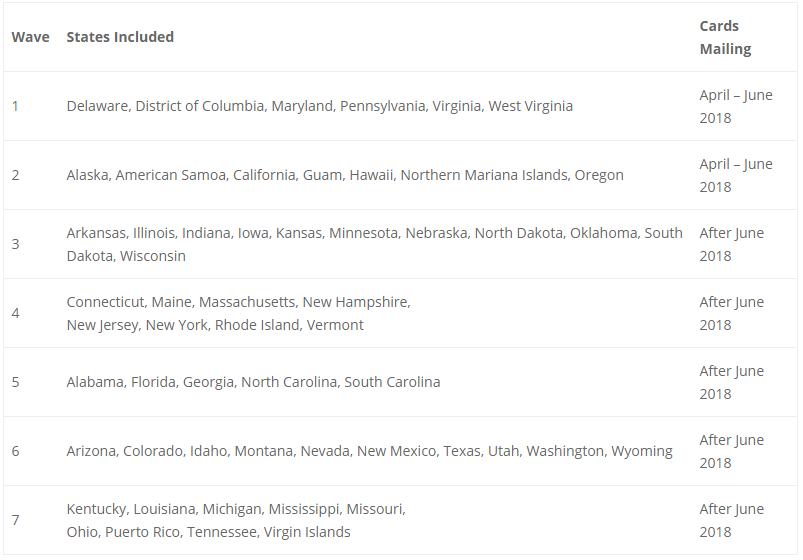
Medicare starts mailing new cards to all enrollees beginning April 2018 in seven geographical waves. Providers can view more information about the phased rollout of the new Medicare cards on the CMS website.
 Systems testing
Systems testing
CMS will test systems that plan to use the MBI. This includes enhanced integration testing (EIT) for new or high risk systems. They are not offering end-to-end testing with Medicare fee-for-service claims processing systems. Providers and payers should be able to use either HICNs or MBIs to submit claims during the transition period.
CMS advises to use the transition period as a live test and make adjustments as necessary, yet still have claims submitted and processed with HICNs until the transition period ends in 2019.
Transition period
Here’s the good news. The transition period extends from April 1, 2018 through December 31, 2019. During this time, providers can use either the HICN or the MBI to exchange data with CMS. CMS will monitor the use of HICNs and MBIs to see how many providers are ready to use only MBIs by January 2020.
Starting January 1, 2020, providers have to submit claims using MBIs (with a few exceptions), no matter what date service was performed. Here are the exceptions listed on the CMS website:
Medicare plan exceptions:
- Appeals
- Adjustments
- Reports
Fee-for-Service claim exceptions:
- Appeals
- Claim status query
- Incoming premium payments
You can get more details for each of these exceptions on the CMS website.
Steps to prepare
To get ready to use the new MBIs, make and internally-test changes to systems and business processes before new Medicare cards are mailed in April. In addition, here are three important tips from the experts at Payor Logic:
- Check the Medicare Learning Network Fact Sheet for details on how to change your systems to accept the new MBI and identify patients who qualify under the Railroad Retirement Board (RBB).
- If you don’t have access to your Medicare Administrative Contractor’s (MAC’s) provider portal, sign up so you can use the provider MBI look-up tool starting in June 2018.
- Attend calls to get more information about this project.
This article was originally published on Payor Logic and is republished here with permission.
