Progress Made in Health IT Adoption
Progress Made in Health IT Adoption
The ONC has released it most recent report to Congress on federal initiatives to advance the process of health IT adoption. Update on the Adoption of Health Information Technology and Related Efforts to Facilitate the Electronic Use and Exchange of Information is an overview of health IT adoption progress from January 1, 2012 to April 30, 2013.
Beyond the hard data, the report describes what steps the ONC and CMS are taking to further health IT adoption and exchange of electronic health information. While the report clearly reflects the tremendous strides made in the last 16 months, it also identifies the barriers providers face in the adoption progress and how various HHS program might help overcome these barriers.
Key findings from the report:
The percent of physicians e-prescribing using an EHR on one of the nation’s largest eprescribing network (Surescripts) increased almost eight-fold from 7 percent in December 2008 to over half of physicians (54 percent) in December 2012.
As of April 2013, more than 291,000 professionals, representing more than half of the nation’s eligible professionals, have received incentive payments through the EHR Incentive Programs. Over 3,800 hospitals, representing about 80 percent of eligible hospitals, and including Critical Access Hospitals, have received incentive payments through this program as well.
In 2009, approximately one in five office-based physicians and one in eight non-federal acute care hospitals had adopted a “basic” EHR withcertain advanced capabilities. By 2012, adoption of “basic” EHRs doubled among physicians and tripled among hospitals; four in ten physicians and over four in ten hospitals had adopted a “basic” EHR system.
Under the ONC Workforce Development Program 17,409 health IT professionals have completed Community College Consortia Program.
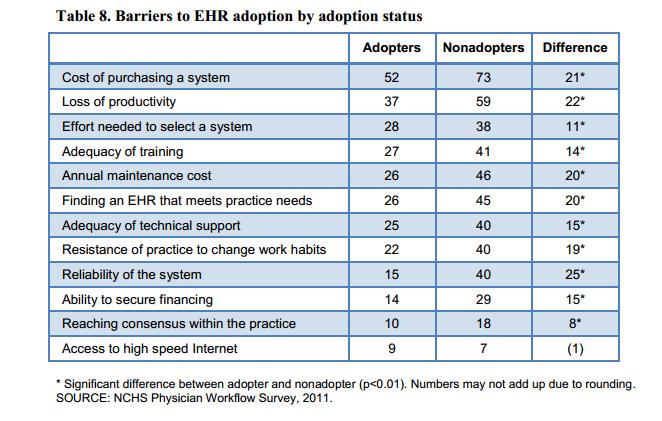
In addressing barriers to EHR adoption, the report identifies the top concerns of office-bases physicians as cost of an EHR system and loss of productivity.
Expanding interoperability capabilities is also addressed. From the report:
While recent years have seen a dramatic increase in the number of U.S. providers using health IT, expanding interoperability remains a challenge. Enabling exchange will involve reducing the cost and complexity of electronic health information exchange, ensuring trust among the key participants of exchange and encouraging exchange of information, particularly during transitions of care.
The report lists four areas in addressing how interoperability in health IT products and systems will be fostered:
- Supporting flexible, incremental, and modular standards
- Selecting standards that work for the future
- Make incremental changes with community feedback
- Supporting implementation and pre-certification testing
Finally, in addressing challenges related to the exchange of health information, the report acknowledges that to date, there has been limited sharing of transitions of care among providers:
ONC recognizes that increasing electronic exchange of health information among providers will involve a multi-pronged approach. Some key challenges perceived by physicians relate to technical barriers, such as the ability of EHR systems to communicate with other systems, the lack of an exchange infrastructure, and the costs of exchanging health information, such as interface costs and transaction fees. In addition to concerns regarding costs and interoperability of EHR systems, providers may not be aware of available mechanisms to electronically exchange health information, including state and local HIE efforts. Furthermore, given that many providers do not currently share health information with other providers during transitions of care, changing providers’ practice patterns or workflow is also needed to increase the electronic exchange of health information—which can be difficult.
The ONC say it will help enable the electronic exchange of health information by:
- Providing mechanisms to exchange health information electronically
- Expanding interoperability of systems
- Reducing the cost and complexity of electronic health information exchange
- Ensuring trust among the key participants of exchange
- Encouraging exchange of health information amongst providers, particularly during transitions of care