 By Sarianne Gruber
By Sarianne Gruber
Twitter: @subtleimpact
What process is used to communicate the medication a patient should be taking? How do you verify that they understand the instructions? Can a healthcare professional provide the most effective communication when educating the Congestive Heart Failure (CHF) patient on medication? The medical and administrative teams at St. Mary’s Hospital in Amsterdam, New York wanted to know the answers to these questions with the objective to reduce CHF readmissions. In many cases, the reason for the readmission is medication non-compliance. One patient will find it easy to “take a pill” daily while another patient is unable to comply the treatment. What can you exactly say to the CHF patient to motivate adherence to the specific medication plan? The research team from iNovum developed a segmentation solution and better yet, helped reduce CHF readmissions. Here is the how the science behind the study works.
A preference-based conjoint analysis was used to define patient attitudes and preferences. The goal was to determine which messages would convince a patient to adhere to a medication plan. First, consider the major silos related to taking medication. Step two, select six classification silos: (1) Education, (2) Cost, (3) Reminders, (4) Quality of Life, (5) Belief and (6) Trust. Step three, create messages as the stand alone pieces of information that communicate attributes and descriptors for taking your medication. Listed in Table 1 are messages related to a Patient’s Belief about Taking Medications.
Table 1. Silo E: Belief about Taking Medications
| Silo E: Belief | |
| E1 | You believe that taking your medication helps your condition |
| E2 | You believe that your medication is safe |
| E3 | You believe that the side effects of your medication are manageable |
| E4 | You believe that the side effects of your medication are tolerable |
| E5 | You believe that your medications do not interfere with each other |
| E6 | You believe that your condition warrants taking your medication |
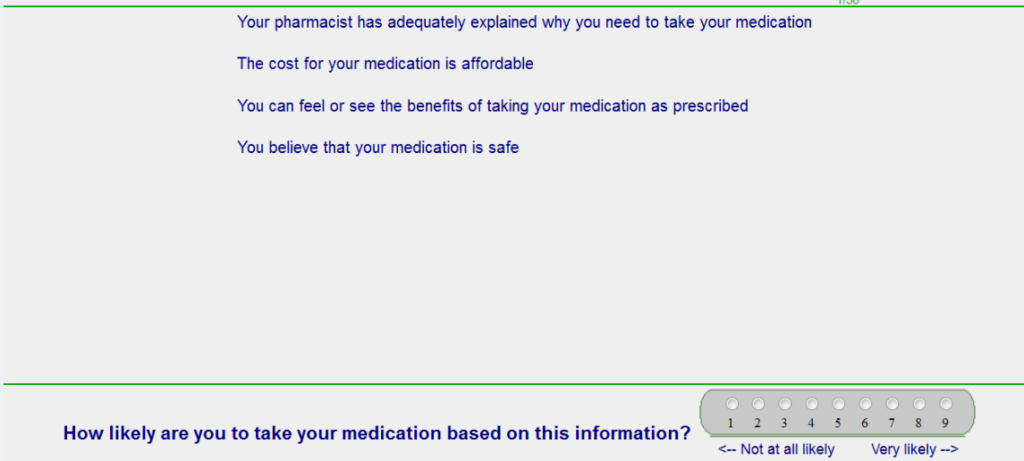
A total of 226 patients participated via the internet. The respondents were tested on a variety of Concept Screens. The study had 6 categories (noted above) and 6 messages per category allowing for 36 unique combinations. A study patient is shown 48 concept screens. For example, the screen below shows 4 messages from 4 categories. These concepts were developed by a systematic combination of the messages via an experimental design and are comprised of 2-4 messages. No two messages from the same silo can appear on the screen at the same time. Messages must appear independently so that the messages are statistically independent of each other so that a regression analysis can be done. For this study, IdeaMap®NET, a patented proprietary optimizer, pulled the viewed messages. Table 2 is the Positioning Page that sets the framework for the study. Table 3 is a Study Sample Screen with a vignette to get the patient’s reaction.
Table 2. Positioning Page
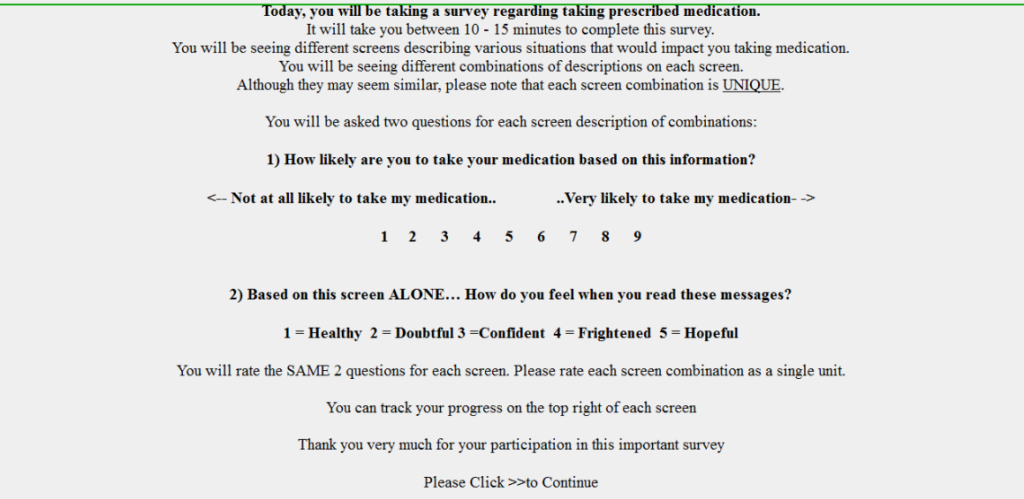
Table 3. Sample Survey Screen
Concept interest scores show the reaction of the patients to the different messages. Concept scores for sample of the 36 messages are shown in Table 4 for the total panel. Here we see a few messages drive compliance on the total sample. Most messages have no effect. And the purple messages should be avoided. The next step is to take a closer look at the sample by using segmentation. Table 5 shows that certain messages are have better appeal within different segments, and that patients’ personal preference perspective is not homogeneous.
Table 4. A Portion of All Tested Messages
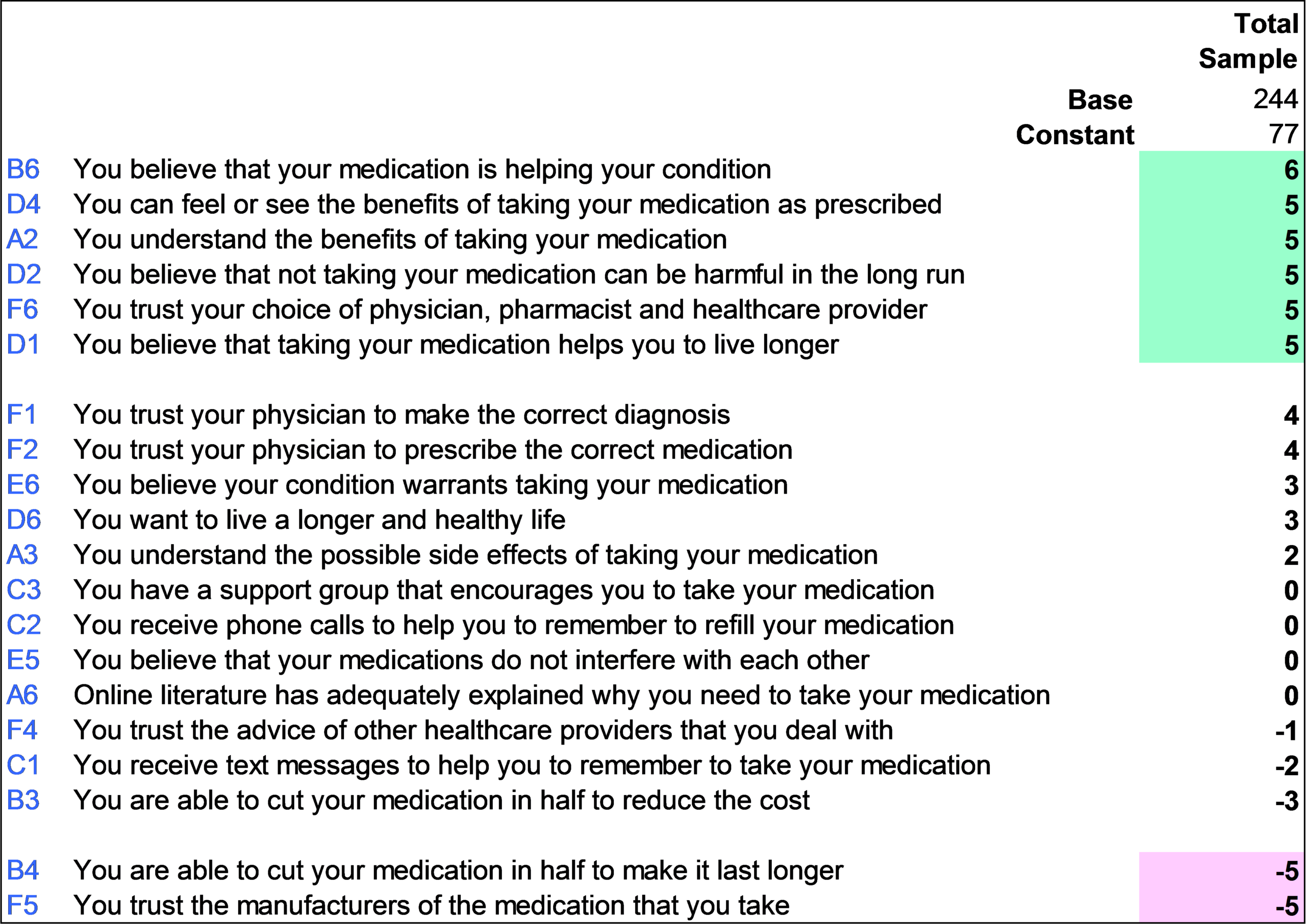
Table 5. Segment 1 – It’s My Decision – Key message: “You have the information and trust what you were told”
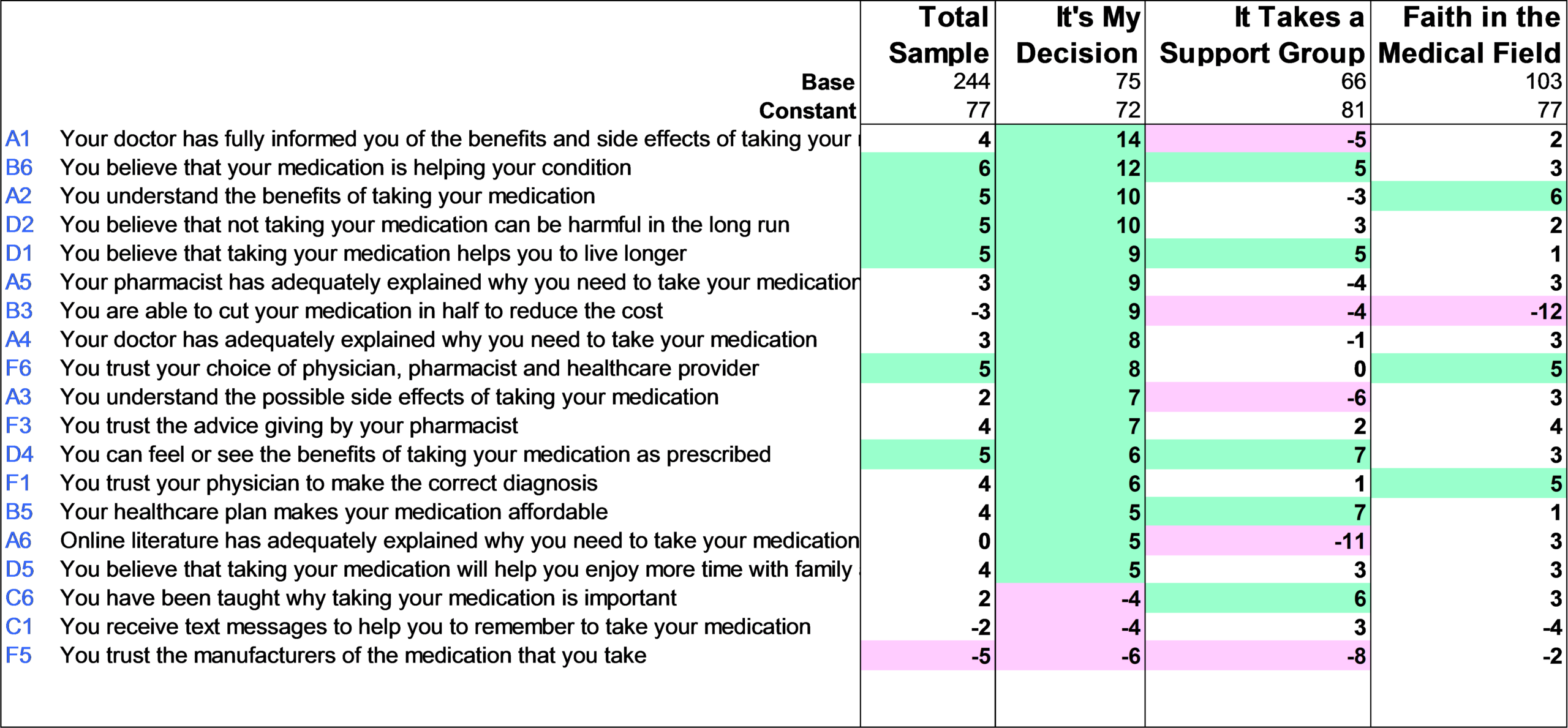
The research at St. Mary’s Hospital uncovered three segments that differentiate patients’ compliance. Segment 1 patients (It’s My Decision) want to retain control and when following instructions. Segment 2 patients (“It Takes a Support Structure”) want to feel that they are not going through this alone and need to have support to motivate them to take their medication. Segment 3 patients (“Faith in the Medical Field”) trust in their medical team given their prior relationships. New patient segment classification is done based on a five question Typing Tool. The CHF medication compliance tool will identify to which Viewpoint Group a patient belongs and subsequently, what programs and messages work best with that patient to help them achieve medical compliance. And most importantly, St. Mary’s Hospital has started to see a decline in readmissions. In 2012, out of a total of 262 non-Inovum patients admitted, 45 patients readmitted within 30 days (17.04%). Compared to 116 inovum segmented patients from February 2013 through June 2013, only 5 patients readmitted within 30 days (3.38%). To cite a staff testimony,” I started the survey with patients, followed the instructions, gave out the handouts, but then something changed”.
