 By Catherine Strawley and Chelsea Richwine, ONC
By Catherine Strawley and Chelsea Richwine, ONC
X: @ONC_HealthIT
Screening for patients’ health-related social needs can help providers more effectively coordinate patient care and connect patients to the resources they need. Social needs are social conditions—such as food insecurity, housing instability, and lack of reliable transportation—which often result from underlying social determinants of health and can adversely affect health outcomes if left unaddressed. While studies show that patients are generally comfortable with social needs screening, little is known about patients’ comfort or preferences around how social needs data are captured and shared with other providers and service organizations to inform treatment and care coordination.
Comfort with Social Needs Data Sharing
Understanding individuals’ comfort with the sharing of their social needs data has implications for patient preferences related to the capture and exchange of potentially patient-sensitive information, particularly with ongoing efforts to increase the collection and use of data on patients’ health related social needs. In recent focus groups of patients, participants expressed a desire for most of their health information to be shareable between providers but indicated sensitivity around data points relating to substance abuse, behavioral and mental health, and social needs. Focus group participants specifically noted that they would be comfortable discussing social needs with providers with whom they had a relationship but would not be comfortable with their information being shared with providers they did not know. They also expressed concerns that this information related to care has been historically stigmatized and could fuel stigma-driven discrimination. Some participants also indicated a lack of trust that their needs could be adequately addressed by their providers because they felt that addressing these needs did not fall within their providers’ scope of work. Despite existing HIPAA protections for these data in a health care context, privacy of information was another major concern contributing to discomfort with social needs data sharing. Taken together, these findings speak to the importance of respecting patient preferences around data sharing and ensuring data privacy.
New data from the 2022 Health Information National Trends Survey (HINTS 6) offers a nationally representative assessment of and an important perspective on individuals’ comfort with providers’ use of data on patients’ health-related social needs. ONC’s analysis of HINTS data shows that while a majority of people —about 60% nationally— were comfortable with their health care providers sharing information about their social needs with other providers for treatment purposes, 4 in 10 individuals nationwide expressed some level of unease with this type of information sharing.
Encouragingly, we found that rates of comfort with social needs information being shared by providers for treatment purposes was not significantly impacted by individuals’ recent experiences with social needs. Those who reported experiencing social needs in the past 12 months indicated they were comfortable with providers sharing their information for treatment purposes at similar rates to those who did not experience these needs (Figure 1).
We did, however, observe differences in comfort with social needs data sharing by individuals’ recent experiences with the healthcare system. For instance, compared to individuals who felt they received very good or excellent quality of care, comfort with each type of social needs information sharing was significantly lower among individuals who reported receiving average or poor care quality (Figure 1). Comfort with information sharing was also relatively low among individuals who reported little or no trust in the healthcare system and among those who experienced discrimination when receiving medical care, but for fewer social needs. Notably, comfort with providers sharing housing concerns was significantly lower among those who received average or poor quality of care, had little or no trust in the healthcare system, and experienced discrimination.
Figure 1. Percent of individuals who reported being comfortable with their providers sharing information about 3 social needs issues (food, housing, transportation), stratified by individuals’ experiences with each social need in the past 12 months, perceived care quality, trust and experiences with discrimination in the healthcare system.
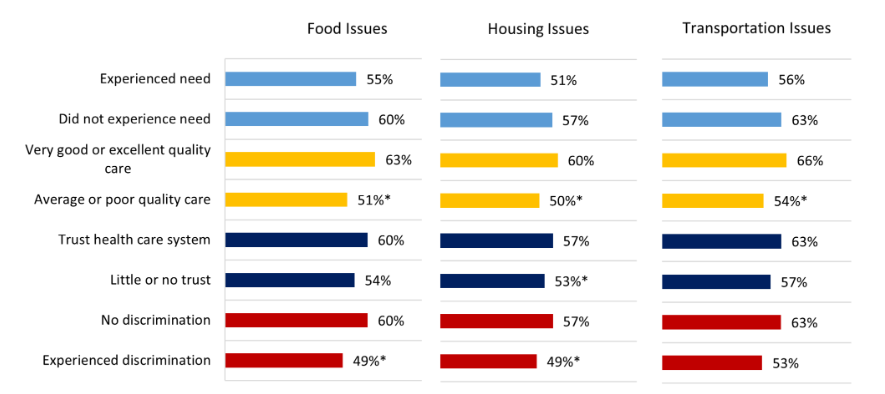
Source: HINTS 6. Notes: * Indicates statistically significant difference from reference group (p < .05).
The Future of Social Needs Data Sharing
Our findings suggest that patient experiences with the healthcare system may influence individuals’ comfort with social needs data sharing between providers for their treatment purposes. This has important implications for providers’ ability to address social needs through a patient-centered approach, as sharing information with other providers or social services organizations is often required to connect patients to the resources or services they need. While a majority of individuals nationwide were comfortable with social needs information sharing, the 4 in 10 Americans reporting some level of discomfort shows room for progress, particularly with respect to underserved populations. ONC’s Social Determinants of Health Information Exchange Toolkit offers guidance on the collection and use of social needs data to facilitate care coordination, including resources on patient consent and privacy. Further, HHS guidance on HIPAA provides details on an individual’s right to request that a covered entity restrict use or disclosure of their protected health information.
As discussions around patient consent continue among academics and policy-making organizations, there may be opportunities for health systems and providers to address patient discomfort with data sharing by addressing well-documented, underlying issues in health care (i.e., poor quality of care, trust in providers or the healthcare system, discrimination) that may contribute to individuals’ discomfort with information sharing. We also know that a large portion of patients are generally concerned about the security of their health information. Therefore, future survey work should evaluate factors, including privacy and security concerns, that contribute to discomfort with social needs data documentation and exchange more directly. Increased transparency around how data will be used and who it will be shared with may help alleviate some of these concerns. Further, ensuring that efforts to increase social needs screening are met with dedicated resources or strategies to address social needs may increase patient confidence that sharing their social needs information will help meet their needs. ONC is committed to ensuring health equity by design in health IT product development, including funding in 2021 to support a UT Austin project focused on refining standards implementation to facilitate smooth and secure referrals and transfer of patients’ care between community-based organizations and health care providers. We hope that this project and similar initiatives will improve the effectiveness of efforts to share social need information for treatment purposes, thereby growing patient confidence in these referral processes.
This article was originally published on the Health IT Buzz and is syndicated here with permission.
