 By Vasilios Nassiopoulos, Hayes Management Consulting
By Vasilios Nassiopoulos, Hayes Management Consulting
Twitter: @HayesManagement
With all the hoopla surrounding the recent announcement that CMS is proposing changes to Evaluation & Management (E/M) codes, you would think the government was eliminating documentation requirements altogether. That couldn’t be further from the truth. While the modest proposal impacting 15 E/M office and outpatient visit codes for Medicare is a step in the right direction when it comes to reducing the documentation burden for physicians, it by no means suggests that you should take your eye off the ball when it comes to monitoring and auditing your coding activity.
Proposal Changes to Watch
The proposed changes to the Medicare Physician Fee Schedule affects the 99201-99215 Office and Outpatient Visit codes to provide a new time-based reporting option. Instead of having to document that more than 50 percent of the visit was face-to-face interaction, physicians can now select a code based on the total length of the visit, without regard to how much of the time was direct patient contact.
The proposal also simplifies the history and examination pieces of the three-point system for determining office visits codes, and allows physicians to select their level of service for both new and established patients using only the medical decision-making (MDM) component.
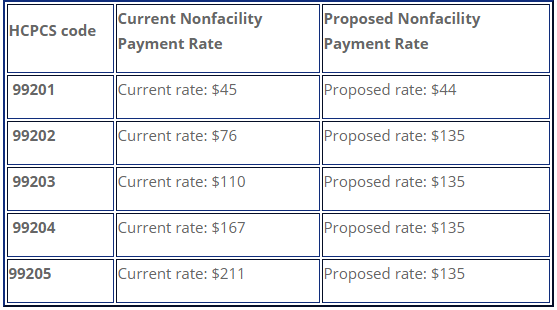
The biggest change alters the current five-level payment plan for new patients (99201-99205) and established patients (99211-99215) from five levels to two. Under the CMS proposal, Level 1 and Levels 2-5 will be paid out at the rates shown below:
Even if the proposal is accepted, there is much that will remain the same. All other E/M services such as inpatient, admissions, consults, critical care, ER, physical and behavioral medicine will remain intact. The 1995-97 coding levels, MDM requirements, and the 99201-99215 codes for diagnoses all remain unchanged.
Remain Vigilant
It’s estimated that the proposed changes could save physicians approximately 50 hours (roughly one week) of documentation time. That’s significant, but it’s important to note that these changes are not final, and if history is any guide, CMS will have to go through a lengthy vetting process that could alter or eliminate some of the changes. Specialty providers are already fighting the financial aspect of the proposal.
Whether or not the changes are approved shouldn’t alter your overall approach to coding compliance. CMS will continue to audit all other codes. The department will still evaluate accurate reporting of MDM that affects quality measures and payments for all E/M codes, including the simplified ones. They will continue to review leveling and apply penalties based on inaccurate or falsified reporting of complexity, which in turn affects case mix indexes and payments.
Fee-for-service payments will continue to be audited for Level 1 vs Level 2 due to the significant payment gap. The importance of appropriate documentation remains high to support medical necessity and complexity. Problems could arise if physicians begin under-coding high-level codes “since payment is the same.” This will result in a false low-complexity patient mix, which will impact profiles and subsequent quality-based payments.
What You Should Be Doing Now
The most appropriate course of action is to continue being proactive when it comes to monitoring your coding documentation compliance. Continue auditing and monitoring all E/M services as you have done in the past.
Here are the steps we recommend:
- Monitor the proposal as it goes through the review process. Historically there will be delays and further changes, but it’s best to prepare for the worst-case scenario.
- Contact vendors that you are using for coding analysis to make sure that they will provide support for the changes should they go into effect in January 2019.
- Prepare as if the changes will happen: Discuss the changes with your coders, begin physician training and anticipate potential software changes to your EMR.
Even though the changes will provide some simplification, the coding levels are not going away. The importance of leveling will continue, as will external auditing from government entities and third parties. It’s important for you to continue to leverage whatever tool you are using to review and audit codes to remain in compliance. If you are not yet using an analytics tool for evaluation, you should consider acquiring one, since the need for such a solution is greater than ever.
Looking Ahead
The good news is that the CMS proposal marks the beginning of a much-needed change of direction to help relieve the documentation burden for clinicians and organizations. Freeing up physicians’ time so they can focus on providing quality care is a positive move. But don’t be lulled into thinking this current proposal will result in a major reduction in documentation. Much of what you’re doing to stay out of the cross-hairs of government regulators and third-party auditors will not change. You still need to be vigilant to avoid costly penalties and reimbursements.
The Hayes team will be staying on top of these changes and sharing our insights on future blog posts, so we can work together to prepare for what’s ahead. Keep reading the Hayes blog for updates!
Read the July 12 CMS announcement.
View the CMS proposed fee schedule.
This article was originally published on Hayes Management Consulting and is republished here with permission.
