A Decade of Data Show that “Sometimes” Isn’t Good Enough
A Decade of Data Show that “Sometimes” Isn’t Good Enough
By Jordan Everson, Wes Barker and Meghan Gabriel, ONC
LinkedIn: Jordan Everson
LinkedIn: Wes Barker
LinkedIn: ONC
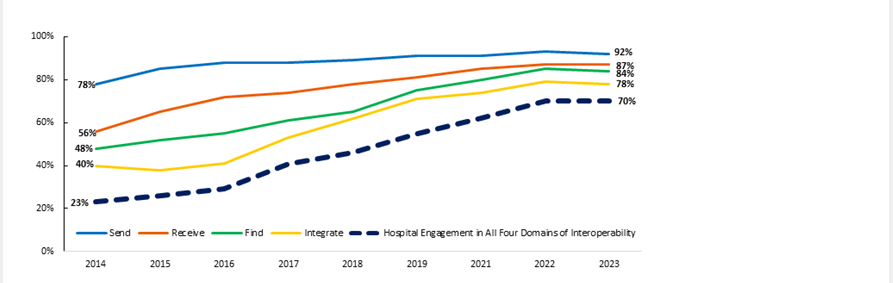
A decade ago, as EHRs were rapidly implemented across the country, ONC sought to make sure these newly implemented technologies were interoperable. Since 2014, ONC has tracked progress toward widespread interoperability among hospitals and physicians by measuring their engagement in four domains of health information exchange: electronically finding, sending, receiving, and integrating patient health information. As shown in the figure below, US hospitals experienced widespread progress toward interoperability with 70% of hospitals reporting that they ‘sometimes’ or ‘often’ engaged in all four domains in 2023, up from 23% in 2014.
Figure 1. Hospitals Engaging in Interoperable Exchange of Electronic Health Information: 2014-2023
Source: American Hospital Information Technology Supplement Survey
While this is a great achievement, we must not rest upon this accomplishment but rather, develop new goals that set the bar higher. This calls for evolving our measurement approach to better capture achievements to come.
Building on a Decade of Interoperability Data
When we first began tracking interoperability, we defined “interoperable exchange” broadly. Hospitals and physicians that either “sometimes” or “often” engaged in finding, sending, receiving and/or integrating patient health information were counted as being engaged in that specific domain of interoperable exchange. We are shifting away from defining interoperable exchange broadly to a more rigorous definition that calls for reaching a higher goal: routine interoperability.
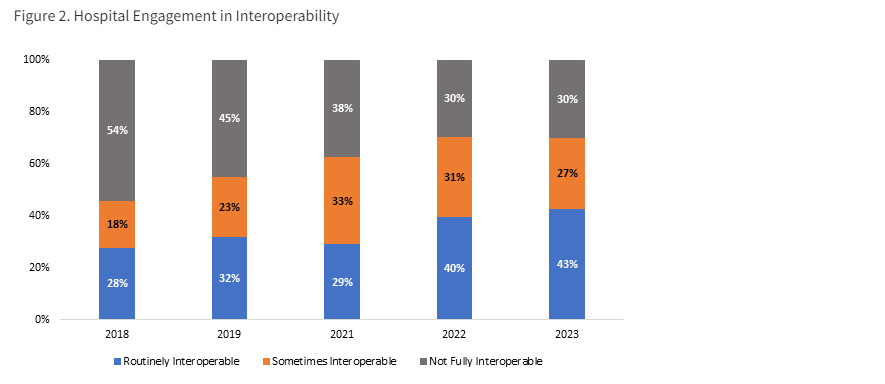
In a new data brief, we split the original metrics for each of the four domains into separate components: one that focuses on interoperable exchange among hospitals that is occurring on a routine basis and another focusing on interoperable exchange occurring sometimes. As shown in the figure below, the overall engagement in all four domains increased from 46% to 70% between 2018 and 2023 based upon the broad definition; however, the more refined metrics allow us to see that the proportion of hospitals that were routinely interoperable overarchingly grew from 28% to 43% of hospitals during the same period.
Figure 2. Hospital Engagement in Interoperability
Source: American Hospital Association Information Technology Supplement Survey
What is the value of these more refined metrics?
When we explore the differences between routinely interoperable hospitals and others, we found that 92% of routinely interoperable hospitals had necessary clinical information available from external providers at the point of care. Comparatively, only 33% of the hospitals that were not routinely interoperable had the necessary clinical information available at the point of care. We also found that routinely interoperable hospitals had greater breadth of exchange with providers across the care continuum, enabling stronger continuity of care, less information gaps, and necessary patient information available at the point of care. This deeper look confirms an underlying point with more precise data – the nation cannot achieve ubiquitous interoperability if certain hospitals continue to only be interoperable “sometimes.”
Defining Success for Physician Interoperability
Increases in physician engagement in interoperability appear to be smaller than increases among hospitals. Data collected since 2015 show only a modest growth in physician engagement in all four domains of interoperability, with a 7-percentage point increase from 2015 to 2021 so that less than one out of 5 physicians engaged in all four domains in 2021. Of note, the physicians that engaged in interoperable exchange of patient health information reported significant benefits; more than 75% indicated electronic exchange resulted in improved practice quality, efficiency, patient safety, and care coordination. This has important implications across the care continuum, particularly behavioral health or long-term care, which also have lower rates of interoperable exchange.
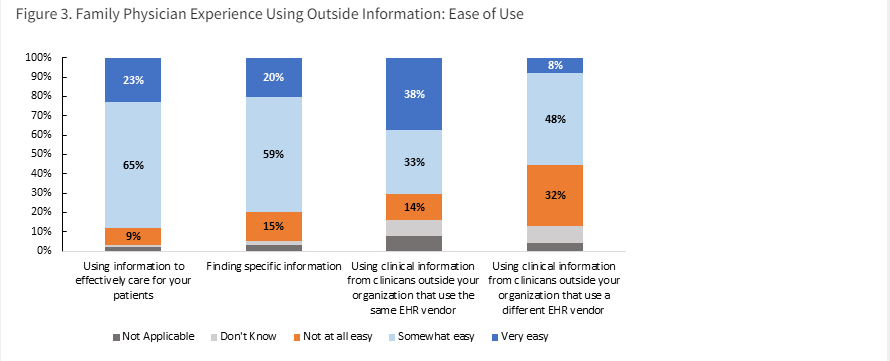
In a recent paper in JAMA Open, which represents a collaboration between ONC and colleagues at the American Board of Family Medicine and the University of California San Francisco, we reported on work to build on our understanding of physician interoperability and downstream impacts of ONC policies on clinicians’ experiences at the point of care. Specifically, in 2022, we assessed family medicine physicians’ satisfaction with how easy it was to use data from external sources. When we took an inclusive approach to defining success by including physicians that said it was either “somewhat” or “very” easy to use information, we found that about 80% stated it was at least “somewhat” easy to use information to effectively care for their patients and find specific information. Approximately 7 out of 10 physicians reported that using clinical information from clinicians outside their organization who use the same EHR developer was at least somewhat easy, and about half indicated that using clinical information from clinicians outside their organization who use a different EHR was at least somewhat easy.
When we raised the bar and focused solely on the highest category of ease of use – “very easy” – we found that only one in five family medicine physicians surveyed reported that it was very easy to use information from outside organizations to care for their patients and to find specific information. And while 38% found it easy to use clinical information from clinicians outside their organization who use the same EHR developer, only 8% reported that using information from clinicians from clinicians who use a different EHR developer was very easy.
Figure 3. Family Physician Experience Using Outside Information: Ease of Use
Source: Primary Care Physicians’ Satisfaction with Interoperable Health Information Technology
Aiming for Routine Interoperability
It is a notable achievement for the nation that we have reached a point where we must raise the bar to meaningfully capture continued progress across all providers in the healthcare continuum. Our future data analyses will continue to emphasize our progress toward the use of interoperable exchange on a routine basis. The data show that health care providers who routinely obtain and integrate information are more likely to have and use the information they need to treat their patients. One in three hospitals report rarely or never engaging in interoperable exchange and physicians predominantly report that it is only somewhat easy to obtain and use clinical information from clinicians outside their organization. Monitoring progress across all aspects of exchange will be important to measure real gains.
As we look towards new policies and programs like continued expansion of the US Core Data for Interoperability (USCDI), USCDI+, and the Trusted Exchange Framework and Common Agreement (TEFCA), we are focused on measuring achievement of widespread, routine, and high value interoperability. It is vital to the nation’s health to establish consistent and reliable sharing of electronic patient health information and ensuring it is useful at the point of care.
This article was originally published on the Health IT Buzz and is syndicated here with permission.