Updated Literature Review Shows that Meaningful Use of Health IT Improves Quality, Safety, and Efficiency Outcomes

Michael Furukawa, Director, Office of Economic Analysis, Evaluation, and Modeling, ONC

Meghan Gabriel, Economist, Office of Economic Analysis, Evaluation, and Modeling, ONC
A new study by RAND researchers found strong evidence that health IT improves patient outcomes.
More and more health care providers are adopting and using health information technology tools like electronic health records (EHRs) since the passage of the Health Information Technology for Economic and Clinical Health (HITECH) Act in 2009. HITECH provided incentives for use of EHRs with functions (‘meaningful use functionalities’) known to enable better care, improved health and lower costs. There is growing anecdotal evidence of the benefits of health IT, but reviews of the evidence base are dated and none have focused on meaningful use functionalities.
That’s why we asked RAND to update previous reviews and examine recent evidence on the effects of meaningful use functionalities on quality, safety, and efficiency outcomes. The study was the largest and most comprehensive assessment of the health IT literature to date.
Meaningful use functionalities have predominantly positive effects on quality, safety, and efficiency outcomes.
- 84% of studies from 2007-2013 reported mostly positive effects of meaningful use functionalities on outcomes (Figure 1).
- Strong evidence supports the use of clinical decision support (CDS) and computerized provider order entry (CPOE).
- Patient access, lists, and reminders had strong positive effects on outcomes; however, the number of studies on these functionalities is relatively small (Figure 2).
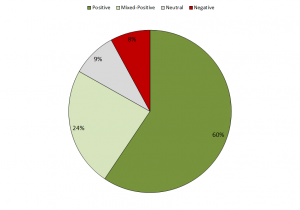 Figure 1: Updated Systematic Review of Effects of Meaningful Use Functionalities on Quality, Safety and Efficiency, By Study Outcome Result (% of Studies)
Figure 1: Updated Systematic Review of Effects of Meaningful Use Functionalities on Quality, Safety and Efficiency, By Study Outcome Result (% of Studies)
Health IT evaluation studies, 2007-2013 (n=493). Positive defined as health IT improved key aspects of care but none worse off; Mixed-positive defined as positive effects of health IT outweighed the negative effects; Neutral defined as health IT not associated with change in outcome; Negative defined as negative effects of health IT on outcome.
Citation: Jones SS, Rudin RS, Perry T, Shekelle PG. “Health Information Technology: An Updated Systematic Review with a Focus on Meaningful Use,” Ann Int Med 2014;160:48-54.
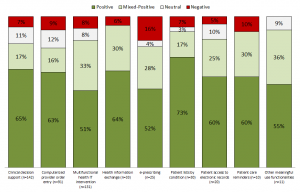 Figure 2: Updated Systematic Review of Effects of Meaningful Use Functionalities on Quality, Safety and Efficiency, By Study Outcome Result (% of Studies)
Figure 2: Updated Systematic Review of Effects of Meaningful Use Functionalities on Quality, Safety and Efficiency, By Study Outcome Result (% of Studies)
Health IT evaluation studies, 2007-2013 (n=493). Number of studies by meaningful use functionality in parentheses. Positive defined as health IT improved key aspects of care but none worse off; Mixed-positive defined as positive effects of health IT outweighed the negative effects; Neutral defined as health IT not associated with change in outcome; Negative defined as negative effects of health IT on outcome.
Citation: Jones SS, Rudin RS, Perry T, Shekelle PG. “Health Information Technology: An Updated Systematic Review with a Focus on Meaningful Use,” Ann Int Med 2014;160:48-54.
Health IT effects varied by type of outcome but were mostly positive overall.
- 78% of health IT studies reported at least some positive effects on safety outcomes.
- More than 75% of studies of health IT alerts and reminders reported positive effects on quality of care.
- 85% of the studies on utilization found that the effects of health IT led to an appropriate increase or decrease in utilization.
The Health IT literature is expanding rapidly.
- Since 1995, more than one-thousand studies on health IT have been published in the peer-reviewed literature, and the number of health IT studies grew by about 25% per year from 2008 to 2012.
- Some meaningful use functionalities, such as CDS and CPOE, have been studied extensively; however, other functionalities related to health information exchange and patient access are not as well-studied.
Future health IT evaluation studies need more details on how context and implementation affect value.
- Reporting on context and implementation was poor, and more than 60% of studies did not report details beyond basic information.
- Researchers should focus on understanding “how” health IT can be used to realize value, and future studies should increase measurement and reporting of context, implementation, and context-sensitivity of effectiveness.
This systematic review included 236 studies published from January 2010 to August 2013. The study also compiled studies from July 2007 to August 2013 and reported outcomes for 493 studies, highlighted in Figures 1 and 2. Details on the methods and detailed findings are reported elsewhere1.
ONC sponsored the study under contract, but the analysis was independently conducted by RAND Health and a technical expert panel.
References
This article was originally published on the ONC’s Health IT Buzz and is republished here with permission. Enlarged images can be seen in original article.
