 By Abhinav Shashank, Chief Executive Officer & Co-Founder, Innovaccer
By Abhinav Shashank, Chief Executive Officer & Co-Founder, Innovaccer
Twitter: @abhinavshashank
Twitter: @innovaccer
What is that one factor that separates one patient from another? Can one identify why two patients with the same illness but from different regions respond differently to a particular treatment? Do we need to cater to the needs of patients even after they leave the clinic?
These questions have always intrigued not only the physicians, but every member who is involved in the care journey— care teams, communities, social workers, even patients themselves. And the answer lies in just one fact— even if these two patients appeared similar on paper, their lifestyles are very likely to differ: socioeconomic status, gender, race, ethnicity, family structure, and education.
All of this comes down to just one term: Social Determinants of Health!
This is one of the prime problems that has kept healthcare organizations in a situation of dilemma.
We are way past the statement that SDOH is just another hype!
Have you ever tried to score a home run with one hand tied behind your back? This situation is similar to the condition of healthcare organizations in the value-based ecosystem. They are trying to get 100% of the task of healing a patient done with just 50% of the insights.
Social determinants matter because they can affect the health of the population residing in a particular region, for better or for worse. We have countless studies that show the importance of social determinants, yet we are not able to properly address them because we are not able to answer these questions:
- How do we address the challenges that we don’t even know exist?
- Who is responsible for addressing these challenges?
Is there any ideal strategy to address SDOH?
No matter how famous they are in healthcare, working with SDOH requires a drilled-down approach and something that we have in abundance- healthcare data. This data can be leveraged, and with the use of predictive analytics, organizations can accurately measure the at-risk population and advance preventive care methods in the ecosystem.
The best way, I think, is to look at this picture with a magnifying glass. Traditionally, the endpoint is the state-level analysis of SDOH. However, it is not the end but the beginning of the study that should go to the zip code level.
Here are some of the most interesting stories of how the leaders in the field of addressing the Social Determinants of Health addressed the populations’ needs and did the undoable.
What was the Humana way to deal with the non-clinical factors?
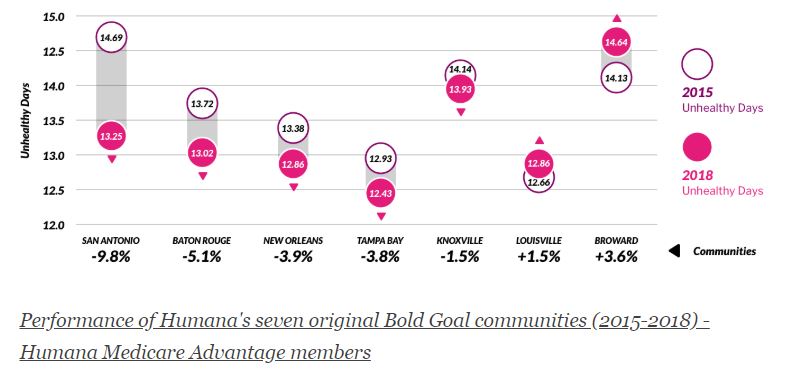
Humana has the Bold Goal Initiative, which is a population health strategy that is aimed at improving the health of the communities and making them 20% healthier by the year 2020. Their Healthy Days surveillance process is a robust and scalable metric. Based on this, they found that food insecurity and loneliness were among the top contributors to the total unhealthy days among the population they serve.
With their holistic and comprehensive approach, they built an analytic intervention pipeline to address these issues. One instance is their intervention with Papa Inc., where they connected college kids to seniors who needed companionship. As a result, 94% of members stated that the Papa Program helped them to feel more socially connected.
Humana was able to reduce the number of unhealthy days from 2015 to 2018 by simply addressing the non-clinical aspects of care delivery for their population.
How MercyOne PHSO took the understanding of non-clinical factors from the zip code level to an individual patient level?
MercyOne PHSO, one of the largest ACOs in the Midwest, wanted to know the factors affecting their patients. They took the simple concept of asking the right questions and leveraged it to understand their patients.
While their patients entered the hospital or examination room, they asked them to complete a survey consisting of questions that depict the factors that affect their patients’ health, such as:
- In the last 12 months, were you worried that your food would run out before you got money to buy more?
- What is your living conditions today?
- Do you face any difficulty in reaching out to your doctor?
… and many more.
In this way, they were able to successfully conduct screening on over 7,000 patients in a year, and were able to identify that food insecurity was among the top domains where their patients needed the most attention.
The road ahead
We are stepping into the age of predicting and preventing diseases instead of curing them. That was the traditional approach. With non-clinical data and resources such as SDOH, we can change the future of healthcare organizations and eventually the US healthcare system.
We just need to look at the bigger picture and the tasks like integrating community resources into the care coordination process or addressing the patient’s need of having someone to talk to could be resolved in just a blink of an eye. All we need is the will to right these wrongs.
This article was originally published on Innovaccer and is republished here with permission.
