This month our reports and surveys didn’t have any overall themes to categorize but mainly interesting information that continues to give a glimpse into where we are going in healthcare. Patients are continuing to take more control of how they want to engage with their healthcare. Will we every see cost under control? Health insurance contracts account for 13% of US gross domestic product, and impose many different administrative burdens on physicians, payers, and patients. And finally is anyone shocked that almost 99% of hospitalized COVID cases are from those who are not vaccinated? A staggering demonstration of how effective the shots have been and an indication that deaths per day could be practically zero if everyone eligible got the vaccine.
Axway Survey Finds Patients Benefit From Healthcare Interoperability but Still Want Better Access to and Ownership of Their Records
Global API Management company Axway (@Axway) released the results from a consumer survey as the new Healthcare Interoperability (CMS) and Patient Access Final Rule roled out July 1. The results showed that while many Americans are taking advantage of growing interoperability in healthcare, they still want more control of their health data.
Nearly All Patients Using Telehealth for Mental Health Care Want to Keep Doing So
As the world shut down from the COVID-19 pandemic, it significantly impacted patients’ mental health and how they connected with their healthcare providers. A new survey by health technology pioneer DrFirst (@DrFirst) examined this impact on 1,000 Americans who had accessed mental health services in the previous year, revealing that over two-thirds feel the pandemic made their mental health worse, and most want to continue using telehealth for mental health visits.
Survey: Only One Quarter Of Nursing Homes Confident They Will Make It Through to Next Year
The American Health Care Association and National Center for Assisted Living (AHCA/NCAL) (@ahcancal), representing more than 14,000 nursing homes, assisted living communities, and other long term care facilities across the country, announced the release of a recent survey of providers across the U.S. Results from the survey showcase the urgent need to address the economic crisis facing the profession.
A Denial a Day Keeps the Doctor Away
According to Becker Friedman Institute (@BeckerFriedman), health insurance contracts account for 13% of US gross domestic product, and impose many different administrative burdens on physicians, payers, and patients. The authors measure one key administrative burden—billing insurance—and ask whether it distorts physicians’ behavior and harms patients. Doctors and insurers often have trouble determining what care a patient’s insurance covers, and at what prices, until after the physician provides treatment. This ambiguity leads to costly billing and bargaining processes after care is provided, what the authors call the costs of incomplete payments (CIP). They estimate these costs across insurers and states and show that CIP have a major impact on Medicaid patients’ access to medical care.
Medical Cost Trend: Behind the Numbers 2022
Each June, PwC’s Health (@PwCHealth) Research Institute (HRI) projects the growth of medical costs in the employer insurance market for the coming calendar year and identifies the leading factors expected to impact the trend. According to the report, health care costs are projected to increase 6.5% in 2022, down from 2021’s 7%. Not suprising because care was canceled or deferred during the pandemic. Other factors include growing mental health issues, preparations for the next pandemic and investments in new digital tools are expected. The report made special note of drug spending as a consistent driver of medical costs.
AP Analysis: Most COVID deaths in US Among Unvaccinated
Nearly all COVID-19 deaths in the U.S. now are in people who weren’t vaccinated, a staggering demonstration of how effective the shots have been and an indication that deaths per day — now down to under 300 — could be practically zero if everyone eligible got the vaccine. An Associated Press (@AP) analysis of available government data from May shows that “breakthrough” infections in fully vaccinated people accounted for fewer than 1,200 of more than 107,000 COVID-19 hospitalizations. That’s about 1.1%.
Yosi Health Survey: Patients Embrace Post-Pandemic Doctor’s Office Changes and Want to See More
Yosi Health (@YosiHealth), a cloud-based, mobile, patient intake, and registration platform released results of a new survey they conducted to gauge patients’ acceptance of doctor office procedures implemented since the COVID-19 pandemic. The survey polled over one thousand people, asking their opinions about the latest health clinic implementations such as telehealth consultations, mobile or kiosk-based contactless check-in, and promptness of their healthcare appointments.
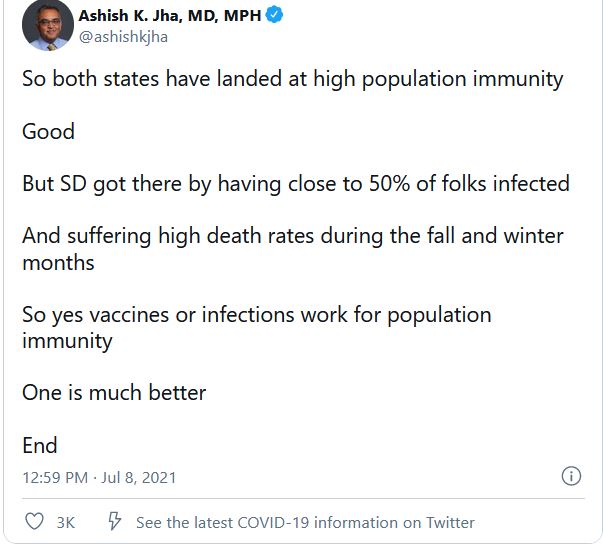
And finally a Tale of Two States
Vermont and South Dakota are actually very similar
Both have slightly older, white, rural populations
Have comparable median incomes
Both have Republican governors
And these days, they look super similar on infections
Here they are over past 2 months
2/5 pic.twitter.com/cMGunE4I3a
— Ashish K. Jha, MD, MPH (@ashishkjha) July 8, 2021
And you can see it in the suffering of the people of the two states
Deaths per capita from COVID in VT vs SD
Nearly 6 times as many folks in SD died from COVID as VT
40/100K in VT versus 230/100K in South Dakota pic.twitter.com/tYsQLfFb3e
— Ashish K. Jha, MD, MPH (@ashishkjha) July 8, 2021