 What “Left Behind” May Look Like
What “Left Behind” May Look Like
By Joy Rios, Managing Partner at Practice Transformation
Twitter: @askjoyrios
According to the 2014 Great American Physician Survey results, 26 percent of providers work as solo practitioners. While EHR adoption has certainly increased significantly in the past several years, as much as 12% have yet to take the digital leap.
Today, I’d like to illustrate the consequences for providers who ignore the EHR Incentive Program, PQRS and, by proxy, the Value-Based Modifier Program. Like it or not, pay for performance is just around the corner and as with most change, ignoring it will not make it go away.
As you may or may not know, CMS phased in the first stages of a national pay-for-performance program-aka the Value Modifier-to groups of 10+ this year. Next year, CMS is proposing to phase the value modifier program to groups of 2+ eligible providers and solo practitioners.
That means that every eligible provider, regardless of group size, will be subject to reimbursement adjustments based on the quality of care metrics that are reported to CMS. When providers choose not to participate in quality reporting programs, whether out of ignorance, negligence, or stubbornness, CMS assumes the worst — that these providers offer their patients poor quality of care at a high cost — and as a result they plan to apply the steepest penalties to their reimbursements.
At this stage of the quality reporting game and going forward, non-action is the most expensive path a provider can take.
Based on 2014 quality measure reporting, penalties of up to 4% will be applied to groups of 10+ eligible providers who do not participate in PQRS. That’s a 2% penalty for PQRS and a 2% penalty for the value modifier.
The proposed rule recommends doubling the value modifier penalty to 4% based on 2015 quality measure reporting, bringing the total penalty related to the PQRS program to 6%. That would be a 2% penalty for PQRS and 4% penalty for the value modifier.
And this number does not include the penalties for not participating in the EHR Incentive program.
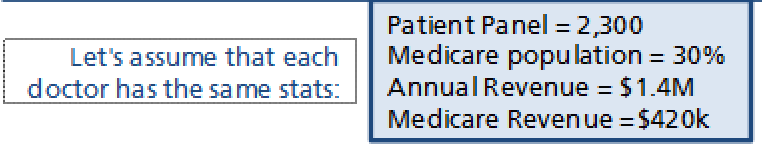
To illustrate the point, I’ve put together a set of scenarios based on the proposed PQRS rule being finalized and the consequences for non-, partial-, and late-participation by three solo practitioners. To ensure that I compare apples to apples, I assumed that each provider:
- sees the same number of patients;
- has the same percentage of Medicare patients;
- has the same annual revenue; and therefore,
- has the same annual reimbursements from Medicare
Like this:
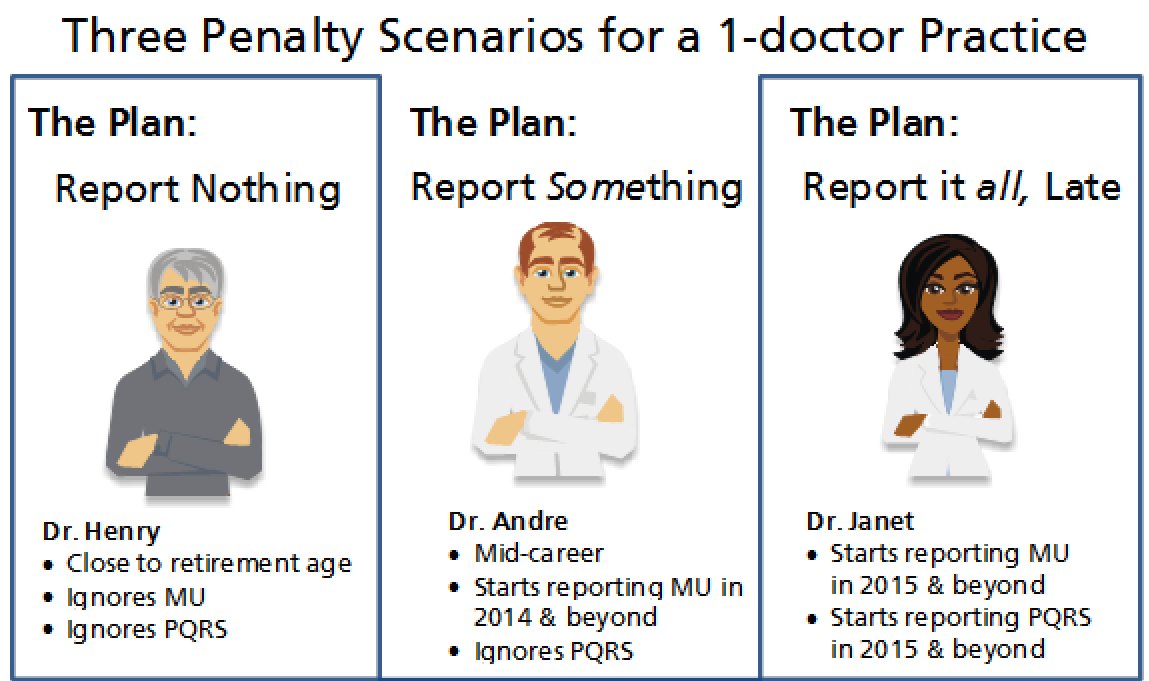
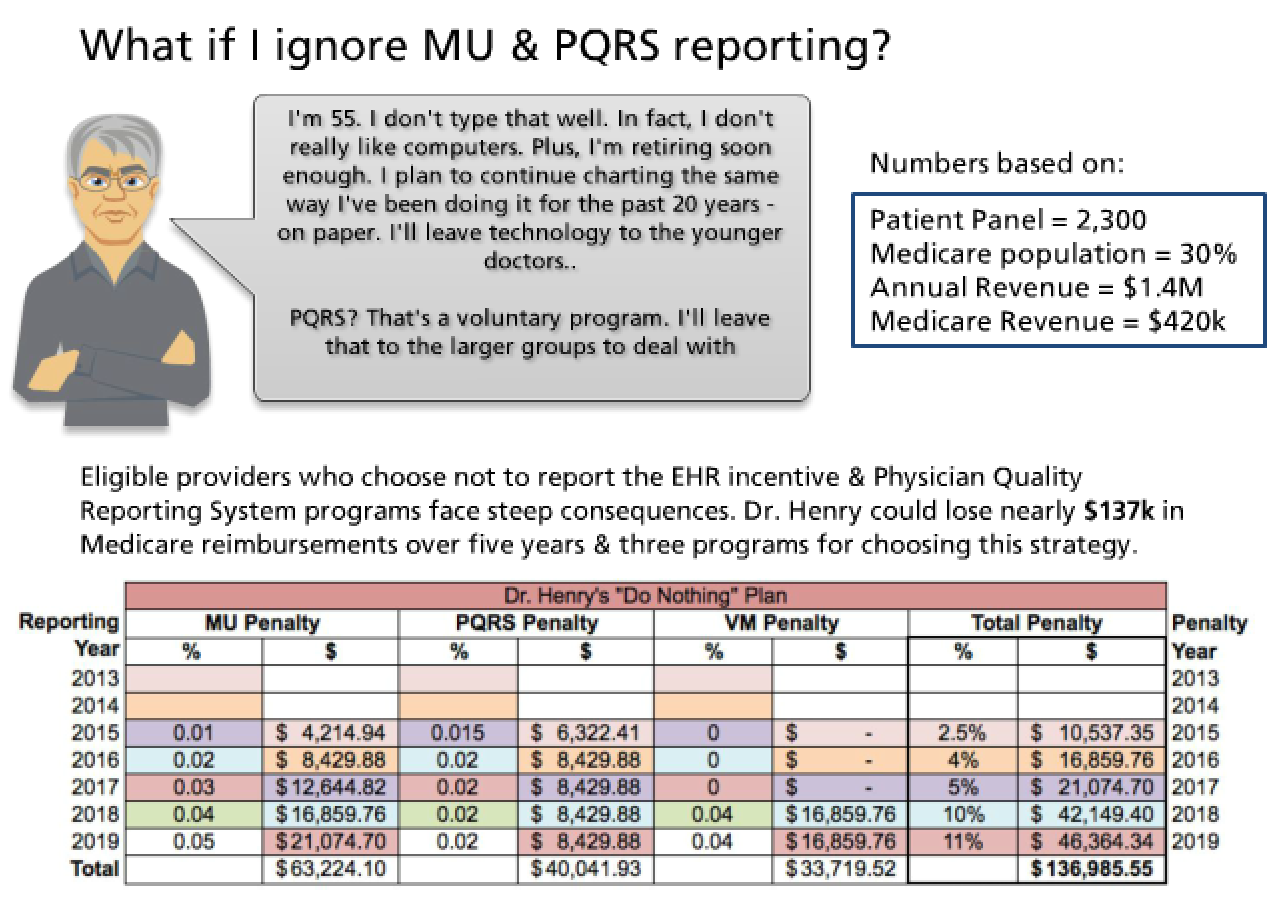
Outlined below are three distinct plans of (non)-action for a solo practitioner. The first provider, Dr. Henry, had decided to ignore both the EHR Incentive Program and PQRS. Dr. Andre, the next example, is getting a late start to the EHR Incentive Program, but will be avoiding PQRS reporting. And lastly, Dr. Janet, is a late bloomer. She will start to report both programs in 2015.
Scenario 1: Report Nothing
Dr. Henry will suffer the highest consequences of this group. Remember that penalties are applied two years after the reporting year, so his first round of negative payment adjustments based on 2013 reporting would result in a $10,500 pay cut in 2015.
Fast forward to the value modifier program being phased in and the penalties become significantly steeper. If he continues his non-reporting of both programs in 2016, he’ll see a $42,000 pay cut in 2018.
Over five years, these penalties add up to nearly $137,000.
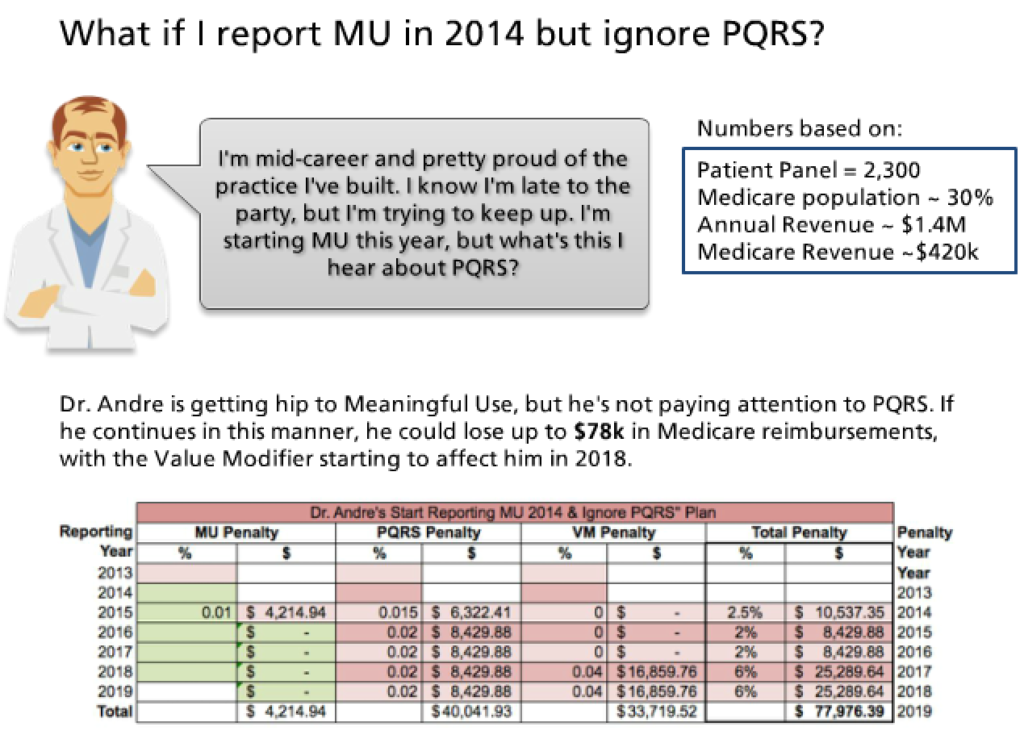
Scenario 2: Report Something
By attesting the EHR Incentive Program in 2014, Dr. Andre will see $59,000 more reimbursements than Dr. Henry, but he will still be significantly impacted by the PQRS and Value Modifier penalties. He’ll lose $40,000 to the PQRS penalty over five years, and nearly $34,000 to the value modifier penalty over the same time period.
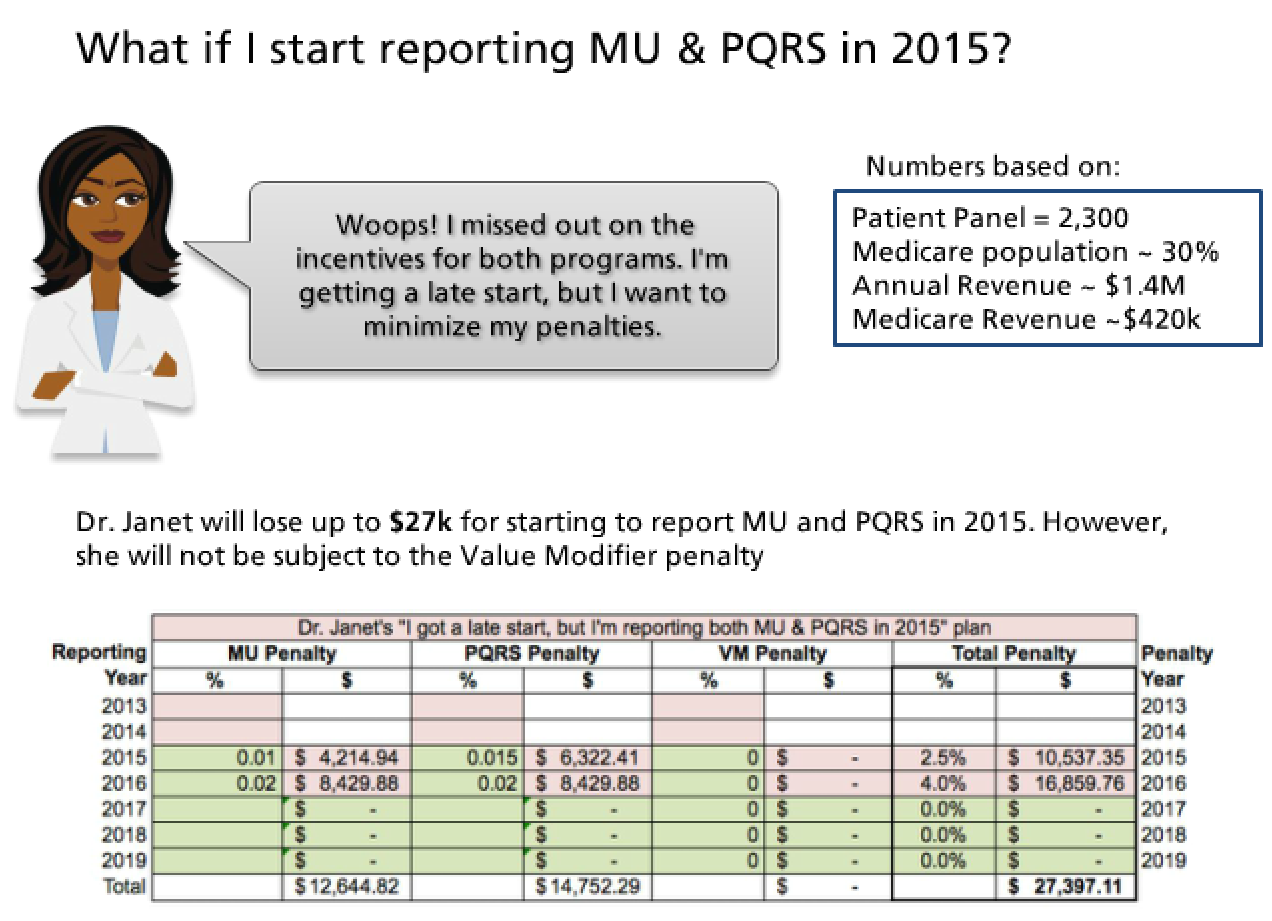
Scenario 3: Report Everything, but Late
Dr. Janet’s non-participation in the programs will cost her about $10,500 in 2015 and about $16,850 in 2016. By starting to report both programs in 2015, she will avoid penalties in 2017 and beyond.
Although these numbers may not be apples-to-apples with your organization, you can see the point — non-action is expensive. What’s your plan?