 By Jeff Jones, Business Project Analyst, GroupOne Health Source Inc.
By Jeff Jones, Business Project Analyst, GroupOne Health Source Inc.
Twitter: @GroupOne_Health
The healthcare industry has unveiled another addition to the already enormous alphabet soup. This new addition goes by the name MIPS, or more properly, Merit-based Incentive Payment System. With the recent “end of Meaningful Use as we know it” announcement by CMS Acting Administrator Andy Slavitt, healthcare providers are scrambling to better understand how MACRA, Meaningful Use, and MIPS will impact their practices.
SGR Repeal and MACRA
The Merit Based Incentive Payment System (MIPS) may routinely be cited under the Medicare Access and CHIP Reauthorization Act of 2015, also known as MACRA. The MACRA act specifically aims to “amend title XVIII of the Social Security Act to repeal the Medicare sustainable growth rate and strengthen Medicare access by improving physician payments and making other improvements, to reauthorize the Children’s Health Insurance Program, and for other purposes” (MIPS Legislation). For the purpose of this blog we will be aiming our focus to the Medicare portions of the legislation.
April 15, 2015 – Congress and President Obama approve one of the most significant and highly bi-partisan bills in the history of U.S. healthcare reform. Nicknamed the “doc fix” bill, aims to repeal the Medicare Part B Sustainable Growth Rate (SGR) reimbursement formula and replaces it with a value-based payment system: MIPS.
To refresh our memories, the Medicare SGR was a method used by Center for Medicare and Medicaid (CMS) to control spending by Medicare on physician services. The SGR was enacted by the Balanced Budget Act of 1997, and replaced the Medicare Volume Performance Standard (MVPS), which was the previous method that CMS used, in an attempt to control costs. This method was to ensure that the yearly increase in the expense per Medicare beneficiary did not exceed the growth in GDP.
Moving to Merit Based Incentives
So how does MIPS plan to succeed in controlling spending by Medicare on physician services, where other pieces of legislation have failed? It plans to utilize three existing programs (Meaningful Use, the Physician Quality Reporting System, and the Value-Based Modifier (VM) Program) and one new program (called Clinical Practice Improvement).
In short, MIPS consolidates and strengthens the financial impacts of these programs, while continuing their performance measurement and reporting mechanisms that have become familiar to providers over the last few years.
How Your MIPS Score Impacts Your Reimbursement
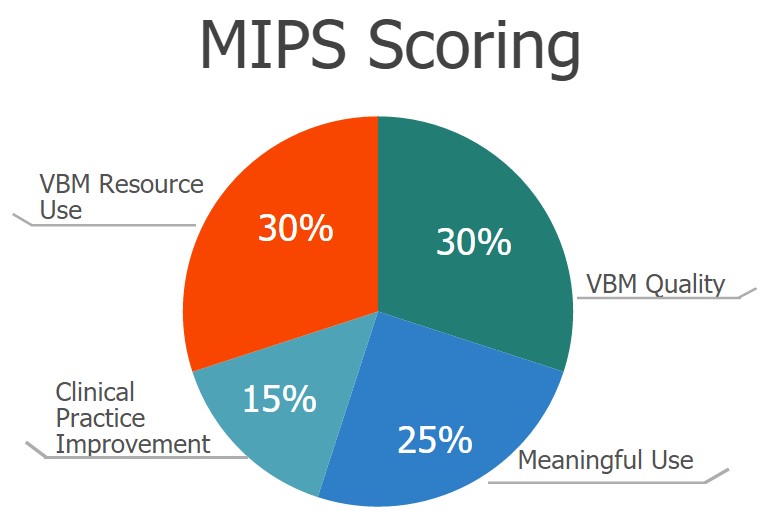
MIPS further goes on to annually measure Medicare Part B providers in these four performance categories to derive a “MIPS score”, from 0 to 100, which can significantly change a provider’s Medicare reimbursements in each payment year. The categories are:
- VBM-measured quality (up to 30 points) – Value-Based Modifier
- VBM-measured resource use (30 points)
- MU (25 points) – Meaningful Use
- Clinical practice improvement (15 points)
The MIPS score’s maximum impact on reimbursement increases from plus or minus 4% for the 2019 payment year to plus or minus 9% for the 2022 and subsequent payment years.
All providers should be familiar with the “performance year” and “payment year” of programs such as Meaningful Use and the Value-Based Modifier Program, where there was a two-year lag between performance and payment years. MIPS will act no differently, meaning the first performance year is expected to be 2017, with MIPS scores then adjusting reimbursements in the 2019 payment year.
Why You Need to Know About MIPS
As you can see MIPS is approaching much sooner than one might think. It is crucial that providers who serve Medicare Part B beneficiaries take the necessary action steps and do their due diligence on MIPS. Even if you do not serve Medicare Part B beneficiaries it is imperative that you begin your research on MIPS now.
Once the big dog (CMS) barks the other dogs (commercial insurance companies) are sure to follow. Meaning the switch from Fee-for-Service to Pay-for-Performance is underway in the healthcare industry, and it goes by the name MIPS.
