 By Kim Boyd, Regulatory Resource Center Lead & Senior Consultant, Point-of-Care Partners
By Kim Boyd, Regulatory Resource Center Lead & Senior Consultant, Point-of-Care Partners
LinkedIn: Kim Boyd
LinkedIn: Point-of-Care Partners
A recent study published in Health Affairs examined the current state of Health Information Organizations (HIOs) and their engagement with the Trusted Exchange Framework and Common Agreement (TEFCA). TEFCA represents a major leap toward creating a unified federal health information exchange (HIE), but the study reveals a mix of optimism and hesitancy across the industry.
You can view the full study here.
Clarifying “Participation”: Becoming a QHIN vs. Joining a QHIN
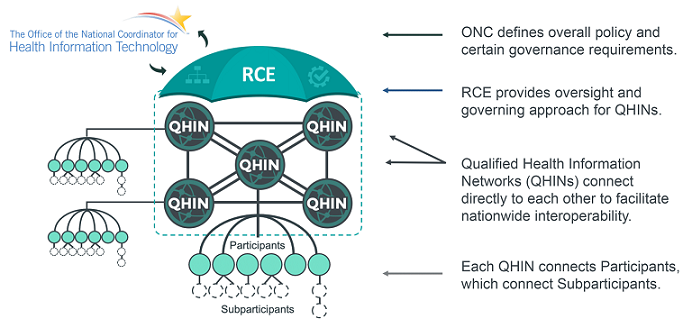
When we talk about participation in TEFCA, it’s crucial to understand what we mean. For Health Information Organizations (HIOs), participation can take two forms: either becoming a Qualified Health Information Network (QHIN) or joining an existing QHIN as a participant.
- Becoming a QHIN is a much higher bar to meet. QHINs are responsible for the large-scale exchange of data across other QHINs, maintaining high standards for interoperability, security, and governance.
- Joining a QHIN as a participant is the more common route for most organizations. Although this role does not carry the same technical and operational burdens as becoming a QHIN, participants must adhere to the rules and standards for secure, interoperable data exchange that are outlined in the Common Agreement.
This distinction is critical because while joining as a participant still involves legal and operational commitments, becoming a QHIN requires far more resources and infrastructure.
Key Findings:
The study highlighted both expected and surprising trends. The number of HIOs has decreased from 119 in 2012 to just 76 in 2023, largely due to consolidation. However, the remaining HIOs are becoming increasingly robust and interconnected with other health networks. Encouragingly, 63% of HIOs plan to participate in TEFCA, marking an increase from 56% in 2019.
However, 32% of HIOs remain uncertain about joining TEFCA in any capacity. This points to a substantial need for greater clarity and education within the sector, especially given the complexity of deciding whether to aim for QHIN status or become a participant.
What Was Surprising vs. Expected:
It was no shock that some HIOs were hesitant to dive into TEFCA due to concerns about costs, resource needs, and the complex nature of integrating new legal and technical frameworks. However, the increasing interest in TEFCA participation, despite these challenges, was somewhat surprising. It seems that the broader industry trend toward interoperability and value-based care is making TEFCA an increasingly attractive option for many.
Challenges & Barriers to Participation:
Several common barriers prevent broader adoption of TEFCA:
- Financial Concerns: Smaller HIOs, in particular, are wary of the costs involved in adapting to the framework, whether as a QHIN or a participant.
- Legal Uncertainty: Concerns about privacy, security, and compliance under the Common Agreement persist.
- Existing Commitments: HIOs with entrenched systems or partnerships are hesitant to disrupt their current models, particularly those already engaged in other data-sharing initiatives.
- Technical Challenges: Interoperability and data integration remain significant hurdles, though those supporting Fast Healthcare Interoperability Resources (FHIR) are more inclined to join as either QHINs or participants.
Cultural Shift: From Proprietary Data to Shared Resource
There’s chatter that some stakeholders, including smaller health systems and organizations, are struggling with TEFCA agreements. This often boils down to a long-standing cultural view in healthcare: data is a proprietary asset, and sharing it means forfeiting revenue opportunities. However, TEFCA—and the broader industry shift—is nudging organizations to reconsider this perspective, encouraging them to view data as a shared resource that enhances patient care. This transition represents a significant cultural change, moving from seeing data as a profit center to recognizing it as a collaborative tool for improving outcomes. As Forbes recently noted, this shift requires organizations to rethink business models that traditionally relied on monetizing proprietary data. You can read more about that shift here.
Similarly, Harvard Business Review emphasizes the need for a well-defined proprietary data strategy to navigate this new landscape. Organizations now face the challenge of balancing the benefits of data sharing with the need to maintain competitive advantage in a rapidly evolving healthcare ecosystem.
The Ever-Present Issue of Data Privacy
Another area of ongoing concern is data privacy and security. During a recent RCE (Recognized Coordinating Entity) call, privacy issues were flagged yet again as a critical factor slowing TEFCA participation. This is not surprising—many HIOs are wary of any initiative that might expose them to new legal risks. TEFCA aims to mitigate these concerns, but privacy, patient matching, and security remain hot-button issues. For more insight, this article by SC Magazine discusses some of the key concerns here.
What Does the Future Hold for TEFCA?
TEFCA is currently voluntary, but there are signs that could change. As the push for nationwide interoperability grows, we may see new regulatory incentives—or even mandates—pushing stakeholders toward participation. The study points to a growing alignment between federal policies and the healthcare sector’s desire for seamless data sharing, which could make TEFCA participation feel inevitable.
Why Should Organizations Participate?
Despite the challenges, there are several compelling reasons for HIOs and other organizations to participate in TEFCA, whether by becoming a QHIN or joining one as a participant:
- Improved Patient Care: Broader data access can lead to more informed and effective patient care.
- Regulatory Alignment: With federal policies increasingly favoring interoperability, TEFCA aligns with where the industry is headed.
- Streamlined Processes: TEFCA can help reduce redundancies and simplify data exchanges across networks.
- Collaboration: Participation opens up new opportunities for collaboration within and across healthcare ecosystems.
Moving Forward: Bridging the Gap
To help more organizations embrace TEFCA, policymakers and the RCE need to consider a more strategic approach to education and support. Offering targeted engagement and practical resources—such as technology upgrade grants and expert consultations—can help HIOs overcome financial and technical barriers. Personalized outreach, one-on-one consultations, and peer-to-peer learning could also make a difference, turning TEFCA from a bureaucratic hurdle into an opportunity for organizations to advance their data-sharing capabilities.
Conclusion
We’re on the cusp of a major shift in how health data is exchanged in the U.S., and TEFCA is a critical part of that journey. The road ahead isn’t easy—there are financial, technical, and cultural challenges to overcome. But with the right support and engagement, TEFCA can lead to a more connected, interoperable healthcare system that puts patients first.
By addressing these barriers through education, support, and incentives, the industry can ensure that HIOs and other stakeholders are well-prepared to navigate this transformation. While voluntary today, TEFCA may soon be an essential part of the healthcare landscape, and those who get ahead of the curve will be best positioned for the future of health data exchange.
This article was originally published on the POCP blog and is republished here with permission.
