 By Jordan Everson and Dan Healy, ONC
By Jordan Everson and Dan Healy, ONC
Twitter: @ONC_HealthIT
In a recent study in the Journal of the American Medical Informatics Association (JAMIA), we leveraged data from the 2020 American Hospital Association (AHA) Information Technology Supplement gathered from April-June 2021, shortly after the initial applicability date of the information blocking regulations (April 5, 2021). We found that 42% of hospitals perceived that at least one type of information blocking “actor” (health care provider, health information network/health information exchange, or health IT developer of certified health IT) engaged in practices that may constitute information blocking. In addition, 36% of responding hospitals reported perceiving that health care providers engaged in information blocking. We also observed important trends where hospitals using health IT developers with smaller national market shares were more likely to report perceived information blocking, as were for-profit hospitals, and hospitals in health care markets where health systems—as opposed to independent hospitals—held large market shares.
New 2022 Data Indicates a Drop in Hospitals’ Observed Perceived Information Blocking by Other Health Care Providers
Recently we published a Quick Stat that updates our analysis with new survey data from the 2022 AHA IT Supplement. The clear takeaway is that a smaller proportion of hospitals reported that health care providers engaged in practices that may constitute information blocking in 2022 (12%) than in 2021 (36%) (Figure 1; full information about these figures is available in the accompanying Quick Stat). In contrast, more hospitals reported experiencing practices that may constitute information blocking by developers of certified health IT in 2022 (22%) than in 2021 (17%).
Figure 1: Percent of Hospitals that Perceived Each Actor Engaged in Possible Information Blocking
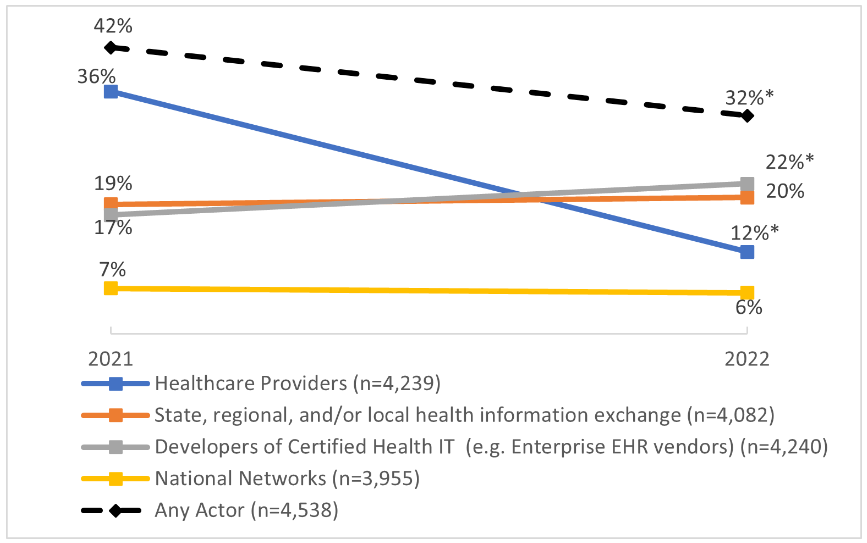
* denotes a statistically significant difference between 2022 and 2021 at p<0.05. Sample sizes correspond to the combined responses for 2021 and 2022, and responses are weighted to reflect the population of hospitals. See Quick Stat for more information about the data source.
A similar trend is evident about two types of health care provider practices that may constitute information blocking. Only 20% of hospitals reported that health care providers used artificial barriers to engage in perceived information blocking in 2022 compared to 35% in 2021. 15% of hospitals reported that health care providers refused to exchange information in 2022, compared with 26% in 2022 (Figure 2).
Figure 2: Percent of Hospitals that Perceived Healthcare Providers Engaged in Three Types of Possible Information Blocking
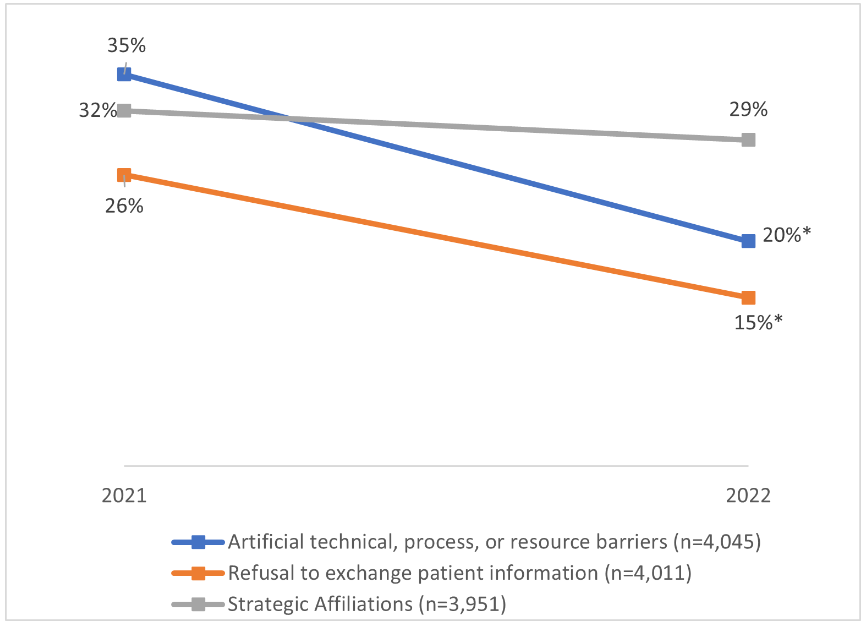
* denotes a statistically significant difference between 2022 and 2021 at p<0.05. Sample sizes correspond to the combined responses for 2021 and 2022, and responses are weighted to reflect the population of hospitals. See Quick Stat for more information about the data source.
Why the Drop?
We think there are three likely explanations for the drop in perceived information blocking among health care providers. First, health care providers have responded to the information blocking rules by changing their practices to reduce possible information blocking. In surveys of health information exchanges in 2015 and 2019, substantially more HIEs reported that developers of certified health IT engaged in information blocking than were reported by hospitals in 2021 and 2022. It might be that developers more quickly adjusted practices in anticipation of the information blocking rule and similar changes by health care providers occurred only after the applicability date. New data from a forthcoming 2023 survey of health information exchanges may support this hypothesis.
Second, hospital leaders may have become more familiar with the specific regulatory definition of information blocking and requirements of the information blocking regulations. With more specific knowledge, those leaders may be realizing that some behavior by health care providers that is frustrating and introduces friction into information exchange does not meet the regulatory definition of information blocking. In contrast, the slightly increasing rates of perceived information blocking by developers may indicate that more specific knowledge is leading hospitals to realize that some developers’ behavior may well constitute information blocking.
Third, the initial data from 2021 may have been an overestimate, and some of the drop we observe may be regression to the mean. It is worth noting that these explanations are not mutually exclusive, and each might be part of the story.
New Data Indicates Few Hospitals that Experience Perceived Information Blocking Report It
Beyond updating data from 2021, the 2022 data also provides important insight into information blocking reports. In response to a new survey question, just 1% of hospital leaders said their hospital had reported perceived information blocking to ONC using the Report Information Blocking Portal. In contrast, 26% of hospital leaders said they had experienced perceived information blocking, but never/rarely reported it, 57% said they did not experience information blocking within the past year, and 15% said they did not know whether their hospital had reported information blocking (Figure 3). That low rate of reporting perceived information blocking aligns with what we see through the portal, where substantially fewer health care providers than patients report perceived information blocking. Infrequent reporting may indicate that this difference is driven as much or more by health care providers under-reporting possible information blocking by others than by the unobserved true rate of information blocking in the field.
Figure 3: Percent of Hospitals that Stated They Reported Perceived Information Blocking on the Report Information Blocking Portal.
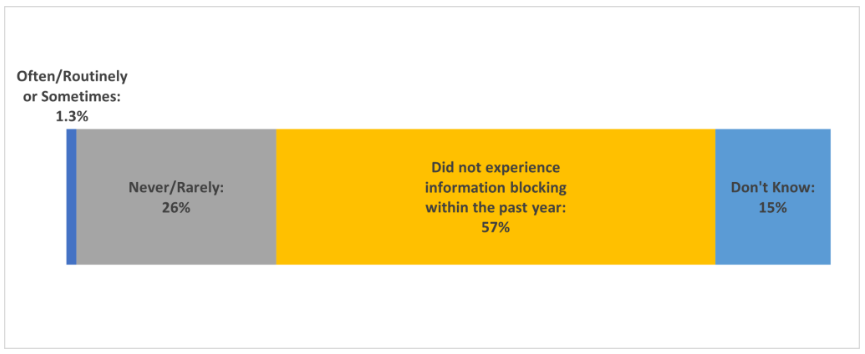
Data represents 2,352 responses to this item from on the 2022 AHA IT Supplement Survey, weighted to reflect the population of hospitals. See Quick Stat for more information about the data source.
Continued Engagement on the Landscape of Information Blocking
Moving forward we plan to continue engaging patients, regulated entities and other interested parties about practices that may constitute information blocking. Information we receive from interested parties across the health care landscape helps inform future educational materials and further engagement around information blocking, including our Information Blocking Claims: By the Numbers Quick Stat, which we aim to update monthly. We also have supported a survey, currently in the field, updating prior surveys on health information exchanges’ perceptions of practices that may constitute information blocking.
We welcome questions, comments, and feedback on information blocking and other health IT topics within ONC’s purview through our Health IT Feedback and Inquiry Portal. Any individual or organization seeking to do so can submit a report of possible information blocking through our Report Information Blocking Portal.
This article was originally published on the Health IT Buzz and is syndicated here with permission.
