 Usability Challenges Remain Unchanged for a Decade
Usability Challenges Remain Unchanged for a Decade
Jacob Reider, MD/ Director, Office of the Chief Medical Officer
The New Year is a time of reflection and anticipation. We reflect on what went well in the past (and perhaps what didn’t go so well); we anticipate future challenges and accomplishments.
As I reflect on the past, I can see that we’ve accomplished incredible things together. The majority of care provided in United States hospitals and medical offices is conducted with the assistance of information technology. Our care is safer, more efficient, and provides research and measurement opportunities that were simply impossible with paper systems.
But as a physician who has used an EHR in my clinical life since 2001, I worry that some of the usability challenges that we early adopters tolerated “for now” (a decade ago) remain unresolved.
This is a problem.
Early adopters of technology are well known to tolerate imperfections. Traditional market forces generally keep products that are difficult to use from succeeding, and as any user of an Apple Newton remembers, the promise of an innovative solution isn’t always realized and will/should fail in the marketplace. Yet some have argued that the meaningful use incentive program altered market forces in a way that prevents well-intentioned products from failing as did Apple’s first “personal digital assistant.” Health IT is not the same as consumer electronics:
a) The user isn’t always the buyer. This causes usability to be a less significant component of buying decisions.
b) Multi-year contracts and technical “lock-in” cause portability to be a true challenge. One can’t just walk away from an EHR that’s not performing as expected. Buying an EHR is more like buying an airplane than a clock radio.
c) Legacy software in a high-risk environment will evolve slowly – for good reason. One can’t change workflow or user experience too quickly, as changes in the user interface can increase error rates even if the new design is better for new users. Errors can harm or kill people. Developers need to evolve user experience slowly and carefully. Usability won’t improve overnight.
d) Health IT systems are complex and require local configuration. Inadequate local resources can cause well-designed products to offer terrible user experiences. To the end-user, they have no way of knowing who is responsible – the IT department or the software developer? Was it Boeing or United Airlines who made these seats so uncomfortable?
Do “I know it when I see it?“ or is there something more complex about enhancing/defining/recognizing usability in Health IT? How does the usability of HIT products have an impact of the quality and efficiency of care delivery? How can we help make HIT products more usable? What is usability?
The (ISO) definition of usability, referenced in the 2009 HIMSS usability primer is a good start:
“Usability is the effectiveness, efficiency and satisfaction with which specific users can achieve a specific set of tasks in a particular environment. In essence, a system with good usability is easy to use and effective. It is intuitive, forgiving of mistakes and allows one to perform necessary tasks quickly, efficiently and with a minimum of mental effort. Tasks which can be performed by the software (such as data retrieval, organization, summary, cross‐checking, calculating, etc.) are done in the background, improving accuracy and freeing up the user’s cognitive resources for other tasks.”
About a decade ago, I was a young(er) family doc, helping physicians in my community learn about how to select and implement an EHR. This was a new domain for them, but they were engaged and enthusiastic. Asked to present the bullet list of criteria that they would use to select the best EHR, I often responded with the list that one would expect:
- Write Notes
- Write Prescriptions
- Write Orders
- Write Messages
- Manage Lab results
But I knew this list wasn’t complete. The missing (and perhaps most important) bullet was usability. Here’s a version of some guidance to my local colleagues circa 2005 that includes the term “usability.” “Are you kidding? Usability?” They asked me after the presentation. “Did you invent a new word?”
In a former life – I had been a software programmer – writing software for the Apple II and then the Apple Macintosh. Apple had a user experience evangelist, and user interface guidelines with which all developers were expected to comply. The guidelines were very clear about the choice of font, order and location of menus, location and position of “help” balloons and so on. Here’s an example of a simple suggestion on how error messages can be more helpful from Apple’s 1995 edition:
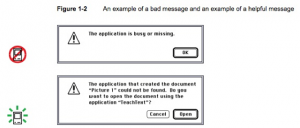 Note that the advice here is to focus on the user. What does the user need to make the best decision?
Note that the advice here is to focus on the user. What does the user need to make the best decision?
While Apple was clearly a pioneer in making computers easier to use, the science of user experience and usability wasn’t new in 1982, and it certainly isn’t new today. Electronic health records are tools that help clinicians do their work, just as websites are tools that help people do work, communicate, etc. Are you developing a website? If so – you can review the great resources available at usability.gov to help you make it more usable.
While the science of user interface design has come a long way since the early 1980′s, the basic principles are the same: focus on the needs and expectations of the person who is using the software. What do they need? When will they need it? How can we help them complete their tasks with the greatest accuracy and the least effort? What are the assumptions that we are making about the user’s workflow or goals?
Consider the expression of lab results. The way that most computer systems report lab results to both providers and patients hasn’t changed in over 20 years. It’s hard for us to tell – at a glance – what’s normal and what isn’t. It’s hard for us to explain to our patients what requires action and what does not. This wired article from a few years ago expresses some of the great opportunities we have to evolve this “last mile” problem in the delivery of information to both providers and consumers.
Obviously, this simple example shows that with extra effort, the abnormal results stand out, making it easier for the provider to take action, and for the patient to understand and collaborate with the provider toward a shared decision.
We know that no software is perfect, and therefore no EHR is perfect. Like the airplane cockpit, the EHR is a complex instrument, to be used by highly trained professionals to perform complex tasks. Any errors in execution of these tasks could be deadly.
Government’s role.
While the usability.gov website provides ample guidance, there is no federal regulation that a website developer incorporate this guidance into their design – nor should there be.
Is health IT different? These systems – if well designed – guide users toward more efficient, safer, better care. If poorly designed, the user may be frustrated or confused, and could make errors that result in patient harm.
Working with experts in the field, we have been guiding the health IT industry toward more consistently incorporating usability into the “bullet list” of expectations above.
- Working with our partners at NIST, we have hosted three annual conferences on usability over the course of the past three years, where we gathered industry experts, health IT developers, provider and patient advocates, and representatives of other federal agencies to learn from each other and provide guidance to the ONC. Artifacts from these meetings are available here.
- ONC’s HIT Policy Committee has hosted two hearings on EHR usability. Here’s a link to the testimony of the hearing in 2010 , and here is a link to the hearing in 2013.
- ONC commissioned the IOM’s report on Health IT and Patient Safety, which includes several recommendations for how health IT usability is an important part of safer care delivery.
- ONC’s 2014 Standard and Certification Criteria include two requirements in the domain of quality management, and usability and safety.
- ONC has funded the work at UT Houston under the SHARP C project to develop:
What’s next?
Enlightened providers like family physician Jeff Belden and “passionate design expert” Stephen Anderson help us think critically about how we develop health IT systems, and question assumptions about the best path forward. As Steve Jobs once said, “it’s not the customer’s job [to figure out how to best design a system].” Belden reminds us that we need to carefully consider the clinician’s native workflow in the optimal design of an EHR process. Anderson’s complex model reminds us that usability is just a milestone along the continuum from functional to meaningful design.
We are working hard to both understand these issues and define an appropriate balance for the government’s role in helping evolve health IT toward better efficiency and safety through enhanced usability. What do you think? We encourage your comments and suggestions.
This article was originally published on the ONC’s Health IT Buzz and is republished here with permission. Enlarged view of image can be seen in original article.
