 By Marilyn Agbeko, Product Marketing Manager, ZirMed
By Marilyn Agbeko, Product Marketing Manager, ZirMed
Twitter: @zirmed
To Repeal or not to repeal; that is NOT the question. Not when it comes value based care and the basic tenets of tying reimbursement to quality. At least, not that we’ve seen yet, and I daresay, not that we will see any time soon. With all the ruckus around repealing and replacing the Affordable Care Act, we have heard little to nothing about MACRA (the Medicare Access and CHIP Reauthorization Act) getting caught in the crossfire. As far as anyone can tell, MACRA, the gateway to Alternative Payment Models (APMs) is here to stay for a while. Accountable Care Organizations, though brought forth by the ACA, are so far avoiding becoming collateral damage as well.
However, don’t focus too much on the vehicles by which risk-based contracts and value based reimbursement structures are enforced – pay attention to the fact that you can no longer avoid participating in some form of an APM. Which means, you have to have the means to deliver and prove high quality of care, and you have to do so while reducing your cost and utilization. Period.
Beyond Legislation
The healthcare industry at large is embracing the concept of value based payments, with Private payers following CMS’s lead and rapidly adopting their own Value based care payment programs such Accountable Care Organizations and Bundled Payments. Humana, as an example, has modeled a bundled payment program not unlike the CMS Comprehensive Care for Joint Replacement (CCJR) program, partnering with organizations that provide hip and knee replacement surgeries. Aetna has multiple ACO agreements with organizations including Memorial Hermann in Houston, Baylor Scott and White in Dallas, Emory Healthcare in Atlanta, Inova in Northern Virginia and many more.¹
Increasing Adoption
In 2015, Leavitt Partners estimated almost 800 Medicare, Medicaid and Commercial ACOs covering over 23 million lives, and projected that number to grow to over 2600 covering 105 million lives by 2020 in the most likely scenario.² Also, CMS has a goal of having 50% of all reimbursements tied to value based APMs by 2018. Cigna, one of the largest payers in the nation, is mirroring CMS’s goal of 50% by 2018 while Aetna’s objective is for 75% of their total spend to be in value based contracts by 2020.
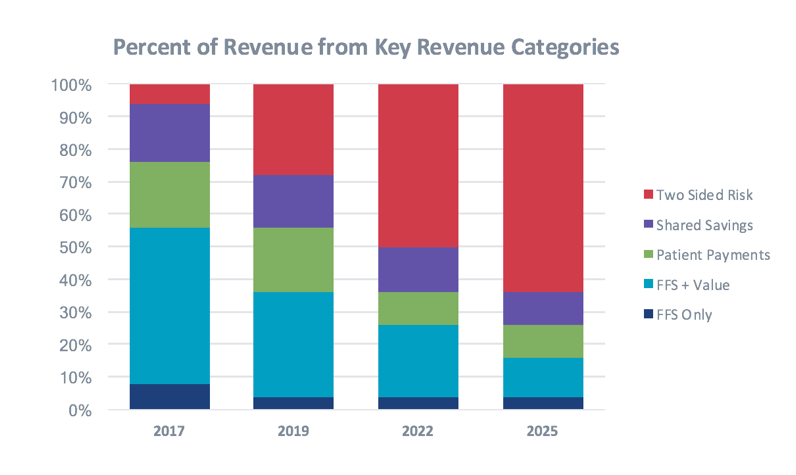
All signs are pointing to accelerated value based reimbursement adoption, with providers seeing more and more of their revenue at risk. And not just the comfortable one-sided risk offered by programs like MSSP – but the uncomfortable, full-skin-in-the-game two sided risk that offers the highest reward potential but also the largest potential pain of lost revenues.
A Riskier Future
In less than 5 years, by 2022 (per our estimates in the graph above), we expect to see more than 50% of payments in some form of a two-sided risk agreement. This includes both CMS and commercial contracts. While we expect to see some providers falling off completely, the remaining providers will need to prepare for the oncoming tide, to ensure a successful transition from Fee for Service to a Fee for Value based payment world.
In our next post, we talk about cutting through the noise and focusing on 4 key elements, which, if managed properly, serve as the base for value based payment models.
¹ Definitive Healthcare
² Leavitt Partners, Projected Growth of Accountable Care Organizations (2015)
This article was originally published on ZirMed and is republished here with permission.
