
By Terry Edwards, President and CEO, PerfectServe
Twitter: @perfectserveCEO
Twitter: @PerfectServe
In a recent survey of nearly 1,000 health system professionals conducted online by Harris Poll and released by PerfectServe, there’s a wide disparity in understanding and opinion between administrative (hospital administrators and office managers) and clinical (physicians, nurses and case managers) respondents on some critical issues.
For example, on the topic of improving population health, administrators say they feel most familiar with their organizations’ strategy, with office managers (95% of the respondents) and hospital administrators (94%) in the know. But clinicians are less familiar with their organizations’ population health strategies – with the exception of case managers (91%), there’s a big drop off when we get to hospitalists (61%), hospital-based specialists (63%) and nurses (65%), who feel least familiar with their organizations’ plans.
This begs several questions: Is there simply a communication or perception gap between the two teams? Is there a strategy that’s well articulated, but uncertainty among those charged with executing it “on the ground” – the clinical community – as to its implementation? Or do clinicians feel they don’t have the tools and systems in place to get the job done?
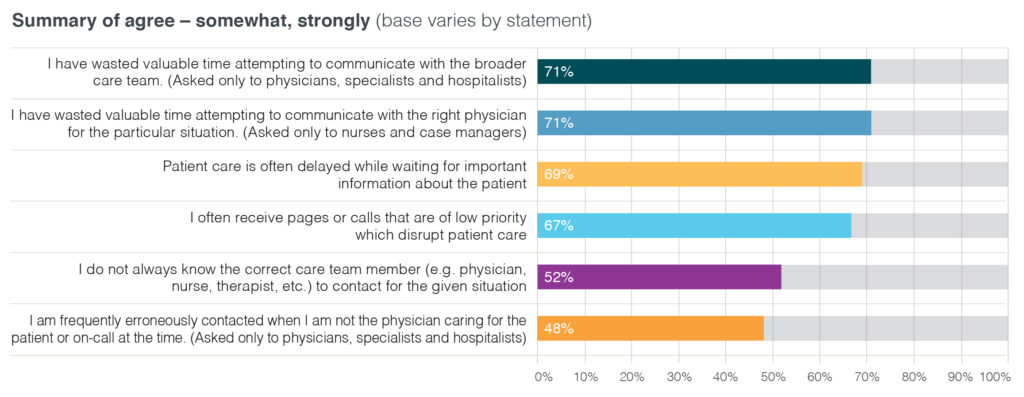
On this last point, clinicians as a whole paint a picture of uncertain communications: 69% feel patient care is often delayed while waiting for important information about the patient, and more than half (52%) admit they don’t know the correct care team member to contact in a given situation. Among the physicians specifically, 71% indicate they have wasted time trying to communicate with the broader care team, and nearly half (48%) report being frequently contacted erroneously when they’re not caring for the patient in question.
 A prescription to fix the system
A prescription to fix the system
Clinical communication could certainly flow more smoothly, and there are a number of means for addressing these issues. Some are fundamental human communication methods; others will require the implementation of secure, communication-driven workflow technology to facilitate timely care team collaboration. Here are some of the measures I see as necessary to improve our transition to population health management:
- Set clear and shared expectations. We need to address the differing opinions between the clinical and administrative sides of the house. This one doesn’t require expenditures for technology or any massive overhauls in workflow or care protocols. Let’s get teams talking about what’s going on. If your organization has a plan for improving population health, and does everyone know what it is? Is it written down? Are there clear, quantitative goals and a baseline of where your organization stands right now? Do clinicians and administration agree on what needs to happen and by when? Has the plan received buy in from all leaders? Does everyone have the tools they need to perform? Care managers may be best suited to act as the go-betweens or the “referees” of the clinical staff, as results from the survey indicate they have the best handle on their organizations’ population health strategies.
- Align efforts and plans. Clinicians express frustration with communications, particularly the question of who is the “go to” for any given situation. My experience suggests this is because clinicians serve in a particular role on a care team, and the person who is in a role can change based upon a number of variables. This is particularly true of handoffs to the next member of the care team or to the outpatient community (PCPs and outside specialists). These interactions require communications technology that enables these workflow processes to save time, effort and lives.
- Provide interoperable secure communications. As much as we’d like the EHR to fulfill this role, it clearly hasn’t (more on that in a future blog post). To avoid clinicians’ taking the path of least resistance and sending an unsecure text or other message that risks a HIPAA violation, we need to give everyone, clinician and administrator alike, a single platform that allows for clear and rapid communication, works with all technologies (including phones and paging) without threatening the integrity of personal health information (PHI). Such a platform will have the longest-lasting effect and impact because it can unify emerging and embedded technologies.
We often talk about getting everyone on the same page. When it comes to clinical communication, this is particularly important. Some improvements will rely on the most basic of activities – discussing the issues and reaching consensus. Once that’s in place, technology can propel improvements the rest of the way to meet the aims of improving population health management.
About the Author: Terry Edwards is the visionary founder, president and CEO of PerfectServe. As chief executive, Edwards has dedicated himself to helping clinicians provide the best and most efficient patient care—while delivering most satisfying customer experience in the healthcare industry. This article was originally published on The Connected Clinician and is republished here with permission.
